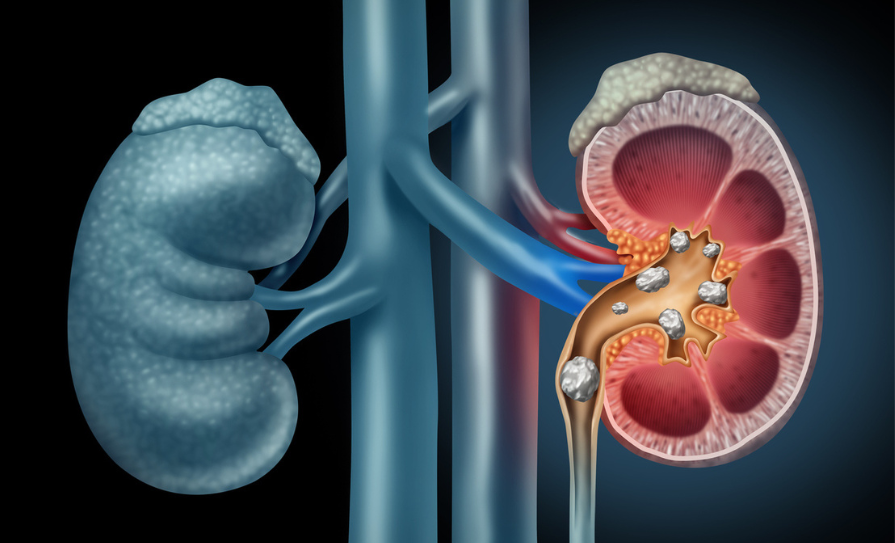
Kidney stones, also known as renal calculi or nephrolithiasis, are solid deposits or crystal aggregations formed in the kidneys from dietary minerals in the urine. They originate in the kidneys but can affect any part of the urinary tract.
Renal calculi affect approximately 12 per cent of the global population, representing a significant cause of morbidity and healthcare burden. The condition is twice as common in males than females, and incidence peaks between 30 and 60 years of age. Recurrence rates are high, with 50 per cent of patients experiencing another episode within five-to-10 years.1,2,3
Once considered a sporadic condition with intermittent exacerbations, nephrolithiasis is now recognised as a complex condition requiring thorough evaluation and multifaceted care. Kidney stones often indicate underlying systemic issues such as metabolic syndrome, genetic disorders, or endocrinopathies.2
Pathophysiology
Kidney stones form through a complex process of supersaturation, nucleation, growth, aggregation, and retention of crystals. There are four primary types of kidney stone:2
- Calcium stones: Comprising about 75-to-80 per cent of stones, they are mainly composed of calcium oxalate and, to a lesser extent, calcium phosphate. Hypercalciuria, hyperoxaluria, and hypocitraturia are key risk factors.
- Uric acid stones: These stones form in persistently acidic urine and are associated with a high-purine diet, gout, and certain metabolic abnormalities.
- Struvite stones: Composed of magnesium ammonium phosphate, these stones are linked to urinary tract infections (UTIs) with urease-producing bacteria. They tend to form large, branching stones called staghorn calculi.
- Cystine stones: Resulting from the genetic disorder cystinuria, these stones are less common and form due to the high concentration of cystine in the urine.
Clinical presentation
The hallmark symptom of kidney stones is renal colic, characterised by sudden, severe pain starting in the flank and radiating to the groin. Other symptoms include haematuria, nausea, vomiting, and dysuria. Some stones may cause intermittent pain or remain asymptomatic until discovered incidentally during imaging for other conditions. Complications can arise if kidney stones obstruct urine flow, leading to hydronephrosis, recurrent UTIs, and chronic kidney disease.1,2,3
Diagnosis
The diagnosis of kidney stones requires clinical evaluation including history and examination, laboratory testing, and imaging studies. Non-contrast helical CT remains the gold standard for imaging, while urinalysis and blood tests provide important insights into the metabolic and systemic factors contributing to stone formation. Comprehensive diagnosis allows for tailored treatment strategies and effective preventive measures to manage and reduce the recurrence of kidney stones.2
History focuses on symptoms, risk factors, and a family history of kidney stones. The clinical history should also include the age of onset for the first stone, number and frequency of episodes, side of the body affected, type of stones formed, type and number of surgical procedures (if undertaken), associated infections, history of gout, obesity, and other metabolic conditions.
The patient’s medications should be considered, as certain drugs can increase the risk of stone formation, including diuretics, calcium supplements, antacids, and antiretrovirals. The history should also include details of dietary habits, particularly regarding fluid intake and output, and consumption of sodium, protein, oxalate, calcium, and sugars.2,3
Physical examination involves assessing the patient for signs of distress due to pain. The abdomen and flank regions should be palpated to identify any tenderness. The patient should also be checked for signs of dehydration and fever, which could indicate a complicated stone or an infection.2,3
Laboratory tests for diagnosing kidney stones include urinalysis to detect the presence of haematuria, pyuria, bacteriuria, and crystalluria. Blood tests are used to assess renal function through measurements of creatinine and estimated glomerular function rate, as well as serum levels of calcium, phosphate, uric acid, and electrolytes. A 24-hour urine collection evaluates urine volume and pH, and measures the excretion of calcium, oxalate, citrate, uric acid, sodium, and creatinine.2,3
Imaging studies primarily include:
- The non-contrast helical CT scan is considered the gold standard for detecting kidney stones due to its high sensitivity and specificity, regardless of the stone’s composition. It provides detailed information about the stone’s size, location, and density. The advantages of this imaging method include its quick execution, widespread availability, and ability to detect other potential causes of abdominal pain.1,2,3
- Ultrasound is preferred for pregnant women, children, and patients requiring frequent imaging to avoid radiation exposure. It is a non-invasive procedure with no radiation risk and can detect hydronephrosis and large stones. However, ultrasound is less sensitive than CT for detecting small stones and ureteral stones.1,2,3
- The kidneys, ureter, bladder (KUB) x-ray is useful for tracking the movement of radiopaque stones, particularly calcium-containing stones, over time. Its limitations include the inability to detect radiolucent stones, such as uric acid stones, and its lower sensitivity for small stones.1,2,3
- Intravenous pyelogram (IVP) involves injecting a contrast dye into the bloodstream, which is filtered by the kidneys and visualises the urinary tract. While it was previously a common diagnostic tool, IVP is now largely replaced by CT due to its superior sensitivity and specificity.1,2,3
- MRI urography is considered for patients who cannot undergo CT, such as those with a contrast allergy or during pregnancy. The advantages of MRI include no radiation exposure and detailed imaging of soft tissues.1,2,3
Differential diagnosis to rule out other conditions includes acute appendicitis, cholecystitis, peptic ulcer disease, diverticulitis, pyelonephritis, and ectopic pregnancy.1,2,3
Treatment and management
The treatment and management of kidney stones requires a multifaceted approach that includes acute management, definitive treatment, and long-term prevention strategies.
Acute management
Renal colic, the severe pain associated with kidney stones, requires prompt and effective pain management. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often the first-line treatment due to their effectiveness in reducing pain and inflammation. They inhibit cyclooxygenase (COX) enzymes, reducing prostaglandin synthesis, thus decreasing inflammation and pain.
Suppositories may be preferred in cases of nausea and vomiting. Paracetamol and opioids are second-line if NSAIDs are contraindicated or insufficient in managing symptoms. Opioids are reserved for patients who do not respond to NSAIDs or have contraindications to their use. They carry a risk of dependence and side-effects, so should be used carefully.2,3
To facilitate the passage of stones, especially those in the ureter, medical expulsive therapy can be used. Alpha-blockers can relax the smooth muscle in the ureter, reduce spasms, and facilitate stone passage, and are particularly effective for distal ureteral stones.
Calcium channel blockers are occasionally used as an alternative to alpha-blockers, to relax the ureteral smooth muscle and aid stone expulsion. Many stones may be observed conservatively, with intervention planned as an outpatient. Smaller stones <5mm have a greater chance (90 per cent) of passing on their own with medical expulsion therapy.1,3,4
Patients with suspected renal colic, with no known history of urinary stones, should be offered urgent imaging. If signs of a possible UTI are present, initial management should include empiric antibiotics, and urine should be sent for culture.3
Hydration is important and increased fluid intake can help flush out smaller stones and reduce the risk of stone formation.3
Approximately 80-to-90 per cent of kidney stones pass on their own. However, about 3 per cent of patients require hospitalisation due to severe pain, inability to pass the stone, sepsis, persistent nausea and vomiting, or dehydration.
Some patients may experience urinary tract obstruction along with an upper UTI, which can lead to urosepsis, pyelonephritis, or obstructive pyelonephritis. In these cases, most patients need an urgent surgical procedure to bypass the stone or drain the renal pelvis until the infection is under control. Once the infection has resolved, elective surgery can be safely performed to remove the stone.1
Definitive treatment
When conservative measures are insufficient, or complications arise, surgical interventions are considered. There are various options for treating elective patients with renal stones, and the decision is based on multiple factors including patient preference; location and size of the stone; comorbidities; and solitary kidney.3,5
Extracorporeal shock wave lithotripsy (ESWL) is indicated for stones that are less than 2cm in size and located in the kidney or upper ureter. The procedure uses shock waves to fragment the stones into smaller pieces that can be passed naturally in the urine.
ESWL is a non-invasive, outpatient procedure with a high success rate for stones that meet the criteria. However, it is less effective for very hard stones, such as cystine stones, and those located in the lower ureter.6
Ureteroscopy is indicated for stones in the ureter or kidney that are not suitable for ESWL. The procedure involves an endoscopic approach that allows direct visualisation and removal or fragmentation of stones using laser lithotripsy. Ureteroscopy has a high success rate and allows for the immediate removal of stones.
However, it requires general or regional anaesthesia and carries a risk of ureteral injury or stricture. Patients are usually routinely stented post-procedure to allow inflammation to settle. These are typically removed one-to-two weeks post-operatively.3,7
Percutaneous nephrolithotomy (PCNL) is indicated for large stones greater than 2cm, complex stones, staghorn calculi, or stones that are not amenable to other treatments. The procedure involves minimally invasive surgery in which a nephroscope is inserted through a small incision in the back to access and remove the stones. PCNL is highly effective for large stones. However, it requires hospitalisation and has a higher risk of complications compared to ESWL and ureteroscopy.8
Open surgery is rarely used and is reserved for cases where minimally invasive techniques fail or are not feasible. The procedure involves a traditional surgical approach to remove stones through a larger incision. This method has a longer recovery time and is associated with higher morbidity.1,2,3
Prevention
Long-term prevention strategies are important to reduce the recurrence of kidney stones. These strategies include dietary modifications, pharmacotherapy, and lifestyle changes.
Dietary modifications are important in managing and preventing kidney stones. Maintaining a high fluid intake is important to ensure a urine output of at least 2-to-2.5 litres per day.3,9 Carbonated drinks should be avoided, and tea/coffee consumed in moderation.
Lowering sodium intake is important to decrease urinary calcium excretion, and reducing animal protein intake helps to lower uric acid levels. Ensuring adequate dietary calcium, rather than supplements, is necessary to bind oxalate in the gut and reduce urinary oxalate levels. Limiting foods high in oxalate (eg, spinach, nuts, tea) helps to decrease urinary oxalate.3,10
Pharmacotherapy plays an important role in the management and prevention of kidney stones. Thiazide diuretics are indicated for hypercalciuria and work by reducing urinary calcium excretion through enhancing renal tubular reabsorption of calcium. Potassium citrate is used for hypocitraturia, uric acid, and cystine stones; it alkalinises the urine and increases urinary citrate, which inhibits stone formation.
Allopurinol is indicated for hyperuricosuria, uric acid stones, and gout, as it reduces uric acid production by inhibiting xanthine oxidase. For cystinuria, cystine-binding agents such as penicillamine and tiopronin are used to prevent stone formation as they form soluble complexes with cystine.1,2,10
Lifestyle changes are important in managing and preventing kidney stones. Achieving and maintaining a healthy weight helps to reduce the risk of metabolic syndrome-associated stones. Obesity is closely related to stone formation.
Engaging in regular physical activity improves overall health and reduces stone risk factors. Regular monitoring through periodic follow-up with urinalysis, blood tests, and imaging is important to detect early recurrence and adjust preventive strategies accordingly.10
Conclusion
Recent advances in the understanding and treatment of kidney stones include the identification of genetic markers associated with increased stone risk, which may lead to future personalised prevention and treatment plans. Research into the role of gut and urinary microbiota in stone formation suggests the potential for probiotic treatments to prevent kidney stones.
Advanced imaging techniques and enhancements such as low-dose CT protocols reduce radiation exposure while maintaining diagnostic accuracy. Dual-energy CT provides improved characterisation of stone composition, aiding in tailored treatment strategies. Innovations in minimally invasive techniques such as advances in flexible ureteroscopy and laser technology have increased the efficacy and safety of endoscopic stone removal procedures.11
Kidney stones are a prevalent and painful condition with significant clinical implications. Advances in diagnostic techniques, medical management, and surgical interventions have improved outcomes. Preventive strategies focusing on dietary and lifestyle modifications, along with pharmacotherapy, are important in reducing recurrence rates. Ongoing research into genetic and microbiome factors holds promise for future personalised treatments and preventive measures.
References
- Leslie SW, Sajjad H, Murphy PB. Renal calculi, nephrolithiasis. [Updated 2024 Apr 20]. In:StatPearls [Internet]. Treasure Island: StatPearls Publishing; 2024. Available at: www.ncbi.nlm.nih.gov/books/NBK442014/.
- Shastri S, Patel J, Sambandam KK, Lederer ED. Kidney stone pathophysiology, evaluation, and management: Core curriculum 2023. Am J Kidney Dis. 2023;82(5):617-634.
- Wilcox CR, Whitehurst LA, Cook P, Somani BK. Kidney stone disease: An update on its management in primary care. Br J Gen Pract. 2020;70(693):205-206.
- Campschroer T, Zhu X, Vernooij RW, Lock MT. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2018;4(4):CD008509.
- National Institute for Health and Care Excellence. Renal and ureteric stones: Assessment and management [Internet]. London: NICE; 2019. Available at: www.nice.org.uk/guidance/ng118/chapter/Recommendations.
- Reesink DJ, Scheltema JMW, Barendrecht MM, et al. Extracorporeal shock wave lithotripsy under intravenous sedation for treatment of urolithiasis. Scand J Urol. 2018;52(5-6):453-458.
- York NE, Zheng M, Elmansy HM, Rivera ME, Krambeck AE, Lingeman JE. Stone-free outcomes of flexible ureteroscopy for renal calculi utilising computed tomography imaging. Urology. 2019;124:52-56.
- Ibrahim A, Wollin D, Preminger G, Andonian S. Technique of percutaneous nephrolithotomy. J Endourol. 2018;32(S1):S17-S27.
- Courbebaisse M, Travers S, Bouderlique E, et al. Hydration for adult patients with nephrolithiasis: Specificities and current recommendations. Nutrients. 2023;15(23):4885.
- Peerapen P, Thongboonkerd V. Kidney stone prevention. Adv Nutr. 2023;14(3):555-569.
- Wang Z, Zhang Y, Zhang J, Deng Q, Liang H. Recent advances on the mechanisms of kidney stone formation (Review). Int J Mol Med. 2021;48(2):149.











Leave a Reply
You must be logged in to post a comment.