Reference: March 2025 | Issue 3 | Vol 11 | Page 31
Hypertension remains one of the most significant global health concerns, contributing to increased risks of cardiovascular disease (CVD), stroke, kidney disease, and overall mortality. Despite advances in detection and treatment, hypertension continues to be inadequately controlled in many populations, contributing to a substantial burden of disease worldwide.1
In August 2024, the European Society of Cardiology (ESC) released updated guidelines on the management of hypertension, reflecting the latest evidence-based strategies to improve patient outcomes.2,3 The guidelines provide refined diagnostic criteria, emphasise more aggressive blood pressure (BP) targets, highlight the importance of comprehensive cardiovascular risk assessment, and introduce novel treatment approaches such as renal denervation for resistant hypertension.2,4,5
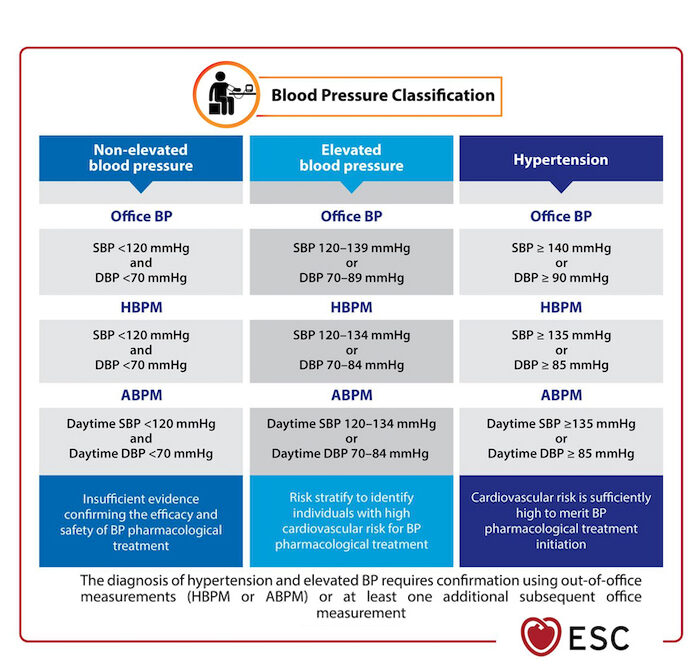
Revised BP classification
The 2024 ESC guidelines introduce a simplified and refined classification system for BP levels. This revision aims to enhance clarity in diagnosis and management while improving communication between healthcare providers and patients. The 2024 guidelines retain the definition of hypertension as a BP of 140/90mmHg or higher. They also establish a new ‘elevated BP’ category for readings between 120-139mmHg systolic and 70-89mmHg diastolic.2,3,6,7
Blood pressure is now categorised into three distinct levels:
- Non-elevated blood pressure is defined as a systolic BP of less than 120mmHg and a diastolic BP of less than 70mmHg. Individuals in this category do not require antihypertensive treatment but should maintain a healthy lifestyle to prevent future increases in blood pressure.2,3,4,6
- Elevated blood pressure is defined
as a systolic BP between 120 and 139mmHg or a diastolic BP between 70 and 89mmHg. While this category does not meet the threshold for hypertension, it signals an increased cardiovascular risk, and the ESC guidelines recommend intensive lifestyle modifications and closer monitoring for these individuals.2,3,4,7 - Hypertension is diagnosed when systolic BP equals or exceeds 140mmHg and/or diastolic BP equals or exceeds 90mmHg. Once diagnosed, hypertension requires structured management that includes lifestyle interventions, pharmacological treatment, and long-term follow-up.2,3,4,7
Intensified BP targets
One of the most significant updates in the 2024 ESC guidelines is the recommendation for more aggressive BP targets.2,3 Evidence from large-scale trials indicates that tighter BP control results in a lower incidence of cardiovascular events such as myocardial infarction, stroke, and heart failure. The guidelines recommend a systolic BP target of 120-129mmHg for most patients on BP-lowering medication, provided the treatment is well tolerated.
For individuals aged 85 years or older, those with symptomatic orthostatic hypotension, moderate-severe frailty, or limited life expectancy, a more lenient approach is advised. In these cases, the goal is to achieve the lowest BP that is practically achievable, as per the ALARA (as low as reasonably achievable) principle.2,3,4,5
To achieve the more intensive blood pressure treatment targets outlined in the guidelines, there is a stronger emphasis on utilising out-of-office BP measurements, such as ambulatory BP monitoring (ABPM) and home BP monitoring (HBPM). These methods are recommended to enhance the accuracy of hypertension diagnosis and management.2,3
Comprehensive cardiovascular risk assessment
Beyond measuring BP alone, the ESC highlight the importance of evaluating overall cardiovascular risk.2,3,4,5 Hypertension does not exist in isolation, but rather interacts with a range of other risk factors that collectively contribute to the development and progression of CVD.7 Recognising this interplay, the ESC guidelines advocate for a holistic approach to risk assessment, ensuring that patients receive comprehensive and individualised care.
Age and sex are important determinants in the development and progression of hypertension. Males and females experience different patterns of BP variation throughout life, influenced by hormonal changes and other physiological factors. Advancing age is also strongly associated with increased arterial stiffness, which exacerbates hypertension and its complications.2,3,4,7
Smoking status is another significant factor, as tobacco use has a profound impact on vascular health. Cigarette smoke contains harmful chemicals that contribute to endothelial dysfunction, leading to increased arterial stiffness, vascular inflammation, and accelerated atherosclerosis. These effects significantly elevate cardiovascular risk, particularly in individuals with hypertension.2,3,4,7
Lipid levels play an important role in cardiovascular risk assessment, as dyslipidaemia significantly increases the likelihood of adverse cardiovascular events in hypertensive patients. Elevated levels of low-density lipoprotein (LDL) cholesterol and triglycerides, coupled with reduced high-density lipoprotein (HDL) cholesterol, contribute to plaque formation within the arteries. This process further narrows the blood vessels, compounding the effects of hypertension and increasing the risk of myocardial infarction and stroke.2,3,4,7
Diabetes mellitus is an independent risk factor for cardiovascular complications and frequently coexists with hypertension. The presence of both conditions amplifies the risk of target organ damage, including the heart, kidneys, and eyes. Patients with diabetes and hypertension require rigorous management strategies to mitigate these risks and prevent long-term complications. 2,3,4,7
A family history of premature CVD is another key element of risk assessment, as genetic predisposition plays a significant role in an individual’s likelihood of developing hypertension. A history of early-onset CVD among close relatives suggests a heightened genetic susceptibility, necessitating proactive screening and early intervention.2,3,4,7
Renal function is intrinsically linked to hypertension, with chronic kidney disease (CKD) both contributing to, and resulting from, high BP. Poorly controlled hypertension can accelerate kidney damage by increasing glomerular pressure, leading to further deterioration in renal function.
Conversely, declining kidney function exacerbates hypertension by impairing the body’s ability to regulate fluid and electrolyte balance. Monitoring renal function is, therefore, an essential component of cardiovascular risk assessment.2,3,4,7
Conducting a thorough and comprehensive risk assessment enables clinicians to tailor treatment strategies to the specific needs of each patient. By considering a wide array of contributing factors, healthcare providers can develop targeted interventions that not only address hypertension but also reduce the overall burden of CVD, ultimately improving long-term patient outcomes.8,9
Lifestyle modifications as first-line therapy
The ESC continues to highlight the fundamental importance of non-pharmacological interventions in the management of hypertension. Lifestyle modifications are recognised as the first-line approach, particularly for individuals with elevated BP who do not yet require antihypertensive medication. These modifications not only help to control BP, but also contribute to overall cardiovascular health.2,3,4,7
Dietary changes play an important role in hypertension management. A diet rich in fruits, vegetables, whole grains, and low-fat dairy products is strongly recommended, while the consumption of saturated fats, sodium, and processed foods should be minimised.
The DASH (Dietary Approaches to Stop Hypertension) diet remains a cornerstone of dietary intervention, as it has been shown to significantly reduce blood pressure levels and lower the risk of cardiovascular events.2, 3, 4,7
Engaging in regular physical activity is another key component of hypertension management. The ESC recommends at least 150 minutes of moderate-intensity aerobic exercise per week, with activities such as brisk walking, cycling, and swimming being particularly beneficial. Regular exercise not only helps lower blood pressure but also improves overall cardiovascular fitness and reduces the risk of other chronic conditions such as diabetes and obesity.2,3,4,7
Weight management is also emphasised, as excess body weight is a major contributing factor to hypertension. Even a modest weight reduction of 5-10 per cent of total body weight can result in significant decreases in BP levels, thereby reducing the risk of hypertension-related complications.2,3,4,7
Alcohol consumption should be moderated to maintain optimal cardiovascular health. The ESC advises limiting alcohol intake to no more than one standard drink per day for women and two for men, as excessive alcohol consumption has been linked to increased BP and a higher risk of CVD.2,3,4,7
Smoking cessation remains one of the most effective strategies for reducing cardiovascular risk in individuals with hypertension. Smoking damages blood vessels, accelerates atherosclerosis, and increases the overall burden on the cardiovascular system. Smoking cessation leads to immediate and long-term health benefits, including improved BP control and a reduced risk of heart disease and stroke.2,3,4,7
By prioritising these lifestyle modifications, individuals with hypertension can achieve better BP control, reduce their reliance on medication, and improve their overall health and wellbeing. The ESC continues to advocate for these non-pharmacological strategies as essential components of comprehensive hypertension management.7
For elevated BP and high CVD risk (high risk CVD conditions or 10-year risk ≥10% or borderline risk of 5-<10% with risk modifiers or abnormal risk tests), lifestyle measures are recommended initially. After three months, if BP remains ≥130/80mmHg, pharmacological BP-lowering treatment is recommended.6
Pharmacological treatment approaches
For patients who do not achieve adequate BP control through lifestyle modifications alone, or who present with significantly elevated BP at baseline, pharmacological therapy is indicated. The guidelines emphasise the importance of combination therapy as the preferred initial treatment approach. This strategy has been shown to enhance BP control more effectively while also improving patient adherence by reducing the complexity of treatment regimens.2,3,7,8
First-line pharmacological agents recommended for hypertension management include several classes of medications, each with distinct mechanisms of action and clinical benefits.
- Angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin II receptor blockers (ARBs) are widely used due to their proven efficacy in reducing cardiovascular risk while also providing renal protection, making them particularly beneficial for patients with conditions such as diabetes or CKD.2,3,9
- Calcium channel blockers (CCBs) are another key treatment option, particularly effective in older adults and those with isolated systolic hypertension, a common condition in ageing populations. Thiazide diuretics are also commonly prescribed, as they help lower BP by reducing blood volume and vascular resistance, making them effective in managing hypertension across various patient groups.2,3,9
- Beta-blockers, while not considered first-line, are recommended in combination with first-line medications when there is compelling indication such as in patients with heart failure, angina, or those recovering from a myocardial infarction, where they provide additional cardioprotective benefits.8
For most individuals requiring pharmacological treatment, a single-pill combination containing two antihypertensive agents is recommended.2,3,7,8 This approach simplifies the treatment regimen and improves medication adherence, ultimately leading to better long-term BP control. In cases where BP remains uncontrolled despite initial combination therapy, the guidelines suggest adding a third agent from a different drug class to further optimise treatment and achieve target BP levels.2,8 By following this structured approach, hypertension management can be more effective, reducing the risk of cardiovascular complications and improving overall patient outcomes.
For patients with resistant hypertension, the 2024 ESC guidelines recommend adding spironolactone (or eplerenone if spironolactone is not tolerated) to the treatment regimen. If blood pressure remains uncontrolled, beta-blockers are suggested as the next option. Additional medications, such as alpha-blockers, hydralazine, or other potassium-sparing diuretics, may be considered. Renal denervation is also an option in certain cases.9
Special considerations in hypertension management
The ESC guidelines provide tailored recommendations for specific patient populations. In older adults, a more cautious approach to BP lowering is advised to minimise the risk of orthostatic hypotension and falls.2,3,4 For patients with chronic kidney disease (CKD), achieving optimal BP control is important, with ACE inhibitors or ARBs being the preferred agents due to their reno protective effects. In individuals with diabetes, BP targets align with those of the general population, but special consideration is given to medications that also provide cardiovascular benefits, such as SGLT2 inhibitors.2,3,4
Patient-centred care and shared decision-making
Recognising the important role of patient engagement in long-term hypertension management, the ESC guidelines note the importance of shared decision-making. Clinicians are encouraged to involve patients in treatment planning, educate them on the importance of adherence, and address potential barriers to compliance. Personalised care strategies improve treatment persistence and overall outcomes.5,7 Encouraging patients to monitor their BP at home is also recommended, and can lead to improved control, greater acceptance of a hypertension diagnosis, increased patient empowerment, and better adherence to treatment.5,7
Gender differences in hypertension
The updated guidelines acknowledge that gender differences influence hypertension prevalence, disease progression, and response to treatment. Women often experience different patterns of BP variation across the lifespan, particularly in relation to menopause. The guidelines encourage personalised approaches that account for these differences to optimise treatment outcomes.2,3,4
Renal denervation for resistant hypertension
A notable inclusion in the 2024 ESC guidelines is the consideration of renal denervation as a potential treatment option for patients with resistant hypertension.2,3,7,10 This non-pharmacological intervention is designed to lower blood pressure by disrupting renal nerve activity, which plays a significant role in the regulation of sympathetic nervous system output and BP control.
The procedure is performed using a minimally invasive catheter-based approach, in which radiofrequency energy or ultrasound is applied to ablate the sympathetic nerves surrounding the renal arteries. By interrupting these nerve signals, renal denervation reduces excessive sympathetic activation, leading to sustained reductions in BP.2,3,7,10
Emerging clinical evidence suggests that renal denervation may be particularly beneficial for individuals who do not achieve adequate BP control despite the use of multiple antihypertensive medications.2,3,4 Several large-scale clinical trials have demonstrated that renal denervation can lead to significant and durable reductions in both office and ABPM.
The procedure appears to be well tolerated, with a low risk of adverse events and no significant impact on renal function. Guidelines emphasise that renal denervation should be performed in centres with the necessary expertise and experience to ensure optimal outcomes.10
Renal denervation is not yet considered a first-line treatment, nor is it recommended for patients with highly impaired renal function, (glomerular filtration rate <40mL/min/1.73m2).10 However, it represents a promising option for carefully selected patients with resistant hypertension, particularly those who struggle with medication adherence or experience intolerable side effects from pharmacological therapy.
Ongoing research continues to refine patient selection criteria and assess the long-term efficacy and safety of the procedure. As the evidence base grows, renal denervation may play an increasingly important role in the management of difficult-to-treat hypertension, offering an alternative or adjunctive approach for achieving optimal blood pressure control.2,3,4
Conclusion
The 2024 ESC guidelines offer a comprehensive and contemporary approach to hypertension management, emphasising individualised care, tighter BP targets, and patient-centred strategies. With a strong focus on lifestyle interventions, combination pharmacotherapy, and novel treatment options, these recommendations are expected to enhance hypertension control and reduce the global burden of CVD.
Healthcare professionals should integrate these guidelines into clinical practice to improve patient outcomes and prevent hypertension-related complications.
Despite the growing number of hypertension guidelines, the rates of diagnosis, treatment, and control of hypertension and elevated BP remain suboptimal. A major factor underlying this is poor implementation of evidence-based guidelines in real-world clinical practice.3
Achieving the ambitious targets set by the 2024 ESC guidelines for hypertension management necessitates effective implementation strategies. A critical first step is to thoroughly understand the obstacles that hinder patients, particularly those in underserved communities, from attaining optimal blood pressure control. While studies such as SPRINT, STEP, and BPROAD have demonstrated the advantages of lower BP targets, additional research is important to determine practical methods for achieving these goals.11
References
- Iqbal AM, Jamal SF. Essential hypertension. [Updated 2023 Jul 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. Available from: www.ncbi.nlm.nih.gov/books/NBK539859/.
- European Society of Cardiology. 2024 ESC clinical practice guidelines for the management of elevated blood pressure and hypertension. Brussels: ESC; 2024 Aug 31. Available at: www.escardio.org/Congresses-Events/ESC-Congress/Congress-news/2024-esc-clinical-practice-guidelines-for-the-management-of-elevated-blood-press.
- McEvoy JW, McCarthy CP, Bruno RM, et al. 2024 ESC guidelines for the management of elevated blood pressure and hypertension. Eur Heart J. 2024;45(38):3912-4018.
- University of Galway. European Society of Cardiology issues new hypertension guidelines. University of Galway; 2024. Available at: www.universityofgalway.ie/about-us/news-and-events/news-archive/2024/august/european-society-of-cardiology-issues-new-hypertension-guidelines-.html#.
- Clinical Practice Guidelines Committee. Essential messages from the 2024 ESC guidelines for the management of elevated blood pressure and hypertension.
Brussels: European Society of Cardiology; 2024. Available from: www.escardio.org/static-file/Escardio/Guidelines/Products/Essential%20Messages/2024%20EM/Essential%20Messages_2024%20HTN.pdf. - McCarthy CP, Touyz RM, McEvoy JW. The ‘10 commandments’ for the 2024 European Society of Cardiology guidelines on elevated blood pressure and hypertension. Eur Heart J. 2024;45(44):4682–4683.
- National Institute for Prevention and Cardiovascular Health. New ESC hypertension guidelines. Galway: NIPC; 2024 Aug. Available at: https://nipc.ie/new-esc-hypertension-guidelines/.
- Badila E. 2024 ESC guidelines for the management of elevated blood pressure and hypertension – how practical is it for clinical practice? Int J Cardiol Cardiovasc Risk Prev. 2024; 23:200341.
- McCarthy CP, Bruno RM, McEvoy JW, et al. 2024 ESC guidelines for the management of elevated blood pressure and hypertension: What is new in pharmacotherapy? Eur Heart J Cardiovasc Pharmacother. 2025;11(1):7-9.
- Lynch P. New ESC hypertension guidelines recommend intensified BP targets. The Medical Independent. 2024 Sep 23. Available at: www.medicalindependent.ie/clinical-news/new-esc-hypertension-guidelines-recommend-intensified-bp-targets/.
- Lu Y, Spatz ES, Krumholz HM. Navigating the 2024 ESC hypertension guidelines: What is new, context, and future directions. J Am Coll Cardiol. 2025;85(5):556–559.
