Reference: February 2025 | Vol 11 | Issue 2 | Page 24
The Global Cancer Statistics (GLOBOCAN) 2020 reports lung cancer to be the current leading cause of cancer-related deaths, with an estimate of 1.8 million deaths globally in 2020.1 Worryingly, more than 80 per cent of patients with lung cancer are diagnosed at an advanced stage, which greatly limits their treatment options and, consequently, results in a poorer prognosis.2
Furthermore, treating patients with late-stage lung cancer is approximately three times costlier for hospitals.3 A large retrospective study reported the per-patient per-month healthcare costs in patients with stage III lung cancer to be over $11,000 (€10,600), and over $21,000 (€20,230) in patients with stage IV disease.3
In patients with an early diagnosis such as those with T1a disease (lesion <1cm), surgical resection is performed, the five-year survival rate of the patient is over 90 per cent.4
In contrast, patients with T4 disease (lesion >7cm or pulmonary lesion <7cm with localised invasion to surrounding structures such as the diaphragm and mediastinal structures) have a five-year survival rate of less than 50 per cent.4
This data demonstrates the importance of diagnosing lung cancer at an early stage. Even when cancer is diagnosed in a timely fashion, another challenge faced by clinicians and patients is the possibility of cancer treatment delay. Delays can occur due to circumstances beyond anyone’s control – a phenomenon that was especially widespread during the Covid-19 pandemic.
Compellingly, a 2020 meta-analysis reported that a four-week delay in cancer treatment was associated with a significant increase in mortality rate among those requiring surgical resection, systemic treatment, or radiotherapy.5
Pulmonary nodules are small growths in the lungs. The majority are benign (due to granulomas or intrapulmonary lymph nodes), with a small proportion of them being pre-malignant or malignant.6 Depending on size, morphology, and patients’ individual risk factors, some pulmonary nodules require follow-up.
However, over 70 per cent of all incidental lung nodules are not followed and managed appropriately.7 This is concerning given that 25 per cent of nodules that require further imaging or investigation have been shown to be of malignant origin.7
In the last decade, lung cancer screening has become more widespread globally, with the US Preventive Services Task Force currently recommending annual low-dose computed tomography (LDCT) screening for lung cancer in adults aged 50 to 80 years who have a 20 pack-year smoking history or more.8
Unfortunately, only 6 per cent of these high-risk patients are participating in yearly screenings.8 Given that early detection of lung cancer is essential in improving cost and patient outcomes, ensuring appropriate detection and follow-up of pulmonary nodules is key.
While lung cancer screening using LDCT has not yet been established in the Republic of Ireland, the lung cancer services in Galway University Hospitals (GUH), led by Dr David Breen, recently collaborated with the Dutch multinational company Philips in using a newly developed software called the lung cancer orchestrator (LCO).
The fundamentals of the software involve identifying abnormal chest X-rays and CT scans performed in one or more institutions by utilising a form of artificial intelligence (AI), called natural language processing (NLP), to screen radiology reports.
NLP involves the application of a wide variety of techniques to process and understand human language. One technique utilised in the LCO involves the detection of keywords in radiology reports. Cases that are identified as ‘abnormal’ by the AI are flagged and brought to the attention of the physician (user) via a work list (Figure 1).
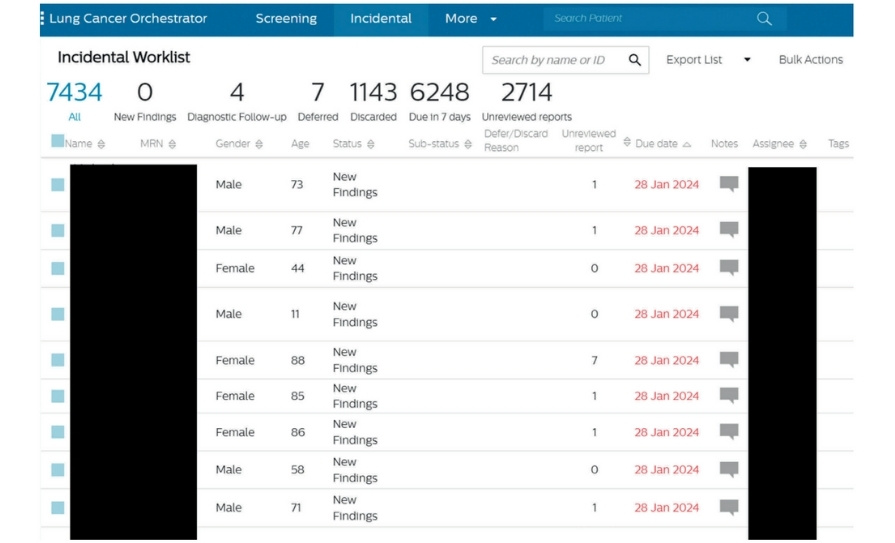
Both images and report can be viewed by the physician, and subsequently can be discarded or listed for further imaging and/or clinical follow-up. Follow-ups of the pulmonary nodules were done in accordance to the Fleischner’s Criteria.9
The need for a lung cancer screening system in GUH was evident following anecdotal reports from several clinicians that patients with incidental pulmonary nodules were inadequately followed up, or in some cases missed being followed up. Furthermore, prior to the introduction of the LCO software to GUH, there were reports of patients who had been diagnosed with advanced lung cancer and who had prior abnormal CTs that had not been followed up.
Given these issues, a virtual incidental pulmonary nodule service was developed that included the introduction of the LCO software with the support of funding from the National Cancer Control Programme. Additional specialist support was obtained from the IT services in GUH, clinical radiology department, and Philips. Following this, a one-year trial was undertaken from 2023 to 2024.
During the trial period, a pre-determined work-flow/protocol was developed and complied with by the screening team (Figure 2). During the one-year trial period, more than 1,000 patients were screened. Over 10 per cent of these patients required further imaging or follow-up, and of these, six patients were eventually diagnosed with lung cancer.
Following the end of the one-year trial and various feedback sessions between the lung cancer team and Philips, it was concluded that the trial was a success and was compatible with the deficits and needs of GUH. It was noted that most cases that were identified by the software would not have otherwise been found or referred to the lung cancer services. Despite the success of incorporating this system, several obstacles and limitations were noted by our team.
Firstly, given the unfamiliarity with the system, the programme was not utilised to its full potential. However, as with every new piece of technology, increased familiarity will allow more advanced features to be utilised.

is automatically moved to a work list

system to pending appointments

(if available) on online system



last known clinician


lung cancer ANP
Appointment arranged for RALC
FIGURE 2: Protocol and work flow for patients identified via the LCO system
Another challenge noted by our team was that the process of screening itself was time-consuming and required substantial administrative support. This could be partially attributed to the fact that the programme was not being utilised to its full potential.
For instance, the hospital’s electronic patient record was not integrated into the system, resulting in a lack of automation. The clinician was often left operating a number of programmes at the time of screening, which reduces the efficiency of the screening process.
In conclusion, utilising Philip’s LCO in GUH as a screening tool was beneficial and can be a good adjunct to pulmonary nodule clinics.
It is also possibly a useful alternative for institutions that do not yet have an established national lung cancer screening programme. GUH has since renewed its licence with Philips for a second year, with plans to further explore the full potential of this programme, such as utilising a function of the software which allows the tracking of individual patients throughout their follow-up pathway, thereby easing the virtual aspect of the care.
References
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209-49.
- https://seer.cancer.gov/.
- Gildea TR, DaCosta Byfield S, Hogarth DK, et al. A retrospective analysis of delays in the diagnosis of lung cancer and associated costs. Clinicoecon Outcomes Res. 2017;9:261-9.
- Kay FU, Kandathil A, Batra K, et al. Revisions to the tumour, node, metastasis staging of lung cancer (8(th) edition): Rationale, radiologic findings, and clinical implications. World J Radiol. 2017;9(6):269-79.
- Hanna TP, King WD, Thibodeau S, et al. Mortality due to cancer treatment delay: Systematic review and meta-analysis. Bmj. 2020;371:m4087.
- Mazzone PJ, Lam L. Evaluating the patient with a pulmonary nodule: A review. Jama. 2022;327(3):264-73.
- Blagev DP, Lloyd JF, Conner K, et al. Follow-up of incidental pulmonary nodules and the radiology report. J Am Coll Radiol. 2014;11(4):378-83.
- Lung cancer screening. National Cancer Institute.
- MacMahon H, Naidich DP, Goo JM, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: From the Fleischner Society 2017. Radiology. 2017;284(1):228-43.