Recently, a new National Clinical Effectiveness Guideline was launched by Minister for Health Simon Harris to help healthcare professionals with the identification, staging and treatment of patients with lung cancer. The new guideline was developed by a group led by the National Cancer Control Programme (NCCP) and was quality assured by the National Clinical Effectiveness Committee (NCEC).
Earlier this year, the NHS also made similar moves in the UK. A National Optimal Clinical Pathway for suspected and confirmed lung cancer has been designed to meet targets as set out in the UK’s Independent Cancer Taskforce report. In addition, it is hoped it will help reduce delays within primary care relating to chest X-ray reporting and referral times with a potential to shorten the time to diagnosis by two to four months.
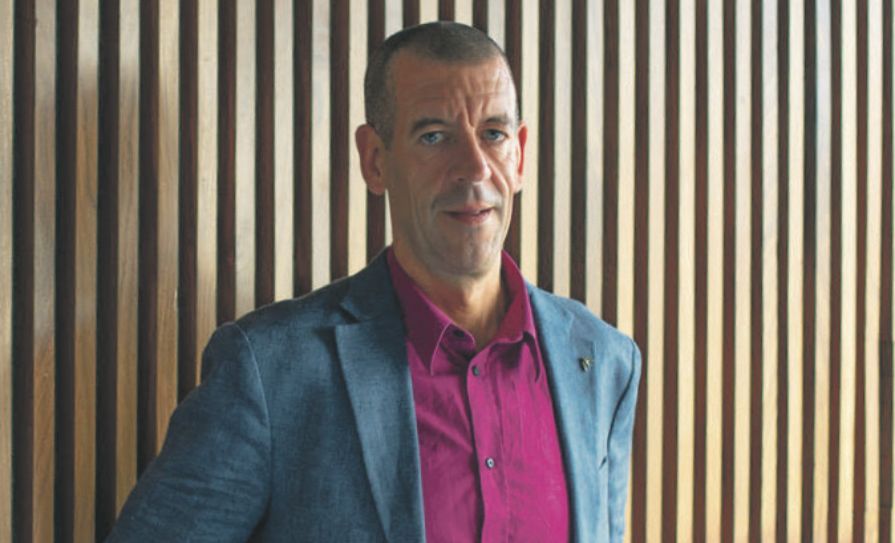
Prof David Baldwin, Consultant Physician with an interest in respiratory medicine at Nottingham University Hospital, UK, spoke at the Irish Thoracic Society Scientific Meeting 2017 on the development of the pathway and its implementation, which is currently taking place throughout the NHS. Prof Baldwin is lead respiratory physician and co-applicant on the UK CT lung cancer screening trial (UKLS), and has written several chapters in well-known respiratory and general medical textbooks and co-edited two books. He has a strong interest in the use of interventional respiratory procedures in the diagnostic and staging process.
Speaking to the <strong><em>Medical Independent</em></strong> (<strong><em>MI</em></strong>), Prof Baldwin said the pathway is “extremely ambitious”.
“If you have a chest X-ray that has been requested by a general practitioner for suspected lung cancer or indeed a chest X-ray that has been requested for any symptoms that could be indicated as suspected lung cancer, that X-ray is reported on the same day preferably,” he explained.
“And preferably a patient has a slot for a CT scan available on the day and they have a clinic appointment if the CT scan is suggestive of lung cancer, on the same day or the next day. Whereas that process would normally take three weeks, it is now going to be compressed into a maximum of five working days. You can report the chest X-ray within 24 hours, but it is preferably within the same day. You can do the CT within 72 hours, but it is preferably on the same day. You can see the patient two days after the CT, so you have got a five-day window to see your patient with a reported CT scan.”
<h3 class=”subheadMIstyles”>Peaks and troughs</h3>
He said managing logistical peaks and troughs will be key if the pathway is to be a success.
“Because the peaks and troughs become more of a problem as your pathway becomes faster, purely because day-to-day you have more peaks and troughs than you have week-to-week, for example,” Prof Baldwin stated.
“So a little more resource is required and you also need to manage the patient because the patient will be going through a very rapid diagnostic process and could become distressed because of that. So we have suggested you need a nurse funded to manage the patient through that process. That is probably the most significant and most challenging part of the pathway because we need radiologists and chest physicians to be able to do things rapidly rather than hanging around for two weeks doing things. So the logistics need to be massively improved so that you process these patients really quickly.”
Prof Baldwin added that improving the manner in which patients are triaged is an important part of the new pathway. Many lung cancer clinics in the UK are full of people who do not actually have the disease so it is necessary to create a robust process whereby patients who have lung cancer, or another serious condition, are prioritised.
“The triage process, which we have been running here in Nottingham for four or five years, came out of the fact that we didn’t have enough clinic slots for lung cancer patients. We have a CT scan, via the chest X-ray to CT route, and the patients that have suggestive CTs of lung cancer go straight through to a lung cancer clinic,” he explained.
“Those that have other cancers will be diverted via another cancer route. Those that have urgent things on their CT scans that need dealing with will be diverted to the other urgent service. Those that have things on their CT scan that could usefully be seen by a chest physician will be booked into a less urgent clinic and have a letter sent reassuring them that the scan doesn’t represent anything serious, but that they would benefit from being seen in a clinic. The ones that have completely normal CT scans and apparently resolved symptoms or minor symptoms on the referral would go straight back to the GP with a letter to the patient and the GP stating ‘everything is ok, but if you do want the patient seen, please get in touch’. That is the triage process. That means it will maximise the value of your clinic slots.”
Prof Baldwin said that for patients who are suitable for curative treatment, or curative radiotherapy, it is important to have all the tests carried out together.
“What you don’t do is request one test and have a look at the result, request another test and look at the result, and then another and so on, and end up delaying the patient massively within the pathway,” he explained.
“That is the ‘radical management bundle’ as we call it. If the patient is not suitable for curative treatment on the CT scan then they just get a biopsy as rapidly as possible, which is sufficient to guide the newly targeted treatments – molecular analysis, etc. The important thing is you can also do a direct-to-biopsy option as well. So if you want a radiologist to do a biopsy immediately after the scan has been done, let them do it, so again you get the diagnosis brought forward massively. We know there are one or two pilots, one in Royal Free Hospital in London, where they do ambulatory lung biopsies; they were doing them on patients that potentially needed further tests afterwards. So what we have tried to do is tailor it so it is only in patients who are unlikely to require a further test afterwards.”
<h3 class=”subheadMIstyles”>Implementation</h3>
The pathway has only recently started to be implemented, even though it was fully developed in January 2016.
“It has taken NHS England a long time to sanction this for reasons only known to themselves,” Prof Baldwin said.
However, prior to official implementation it had been incorporated into the NHS England’s quality assurance measure, meaning many hospitals were well prepared for moving towards the new model. According to Prof Baldwin, although the pathway began being implemented in August, some hospitals are already in compliance with some of its targets.
“We are likely to see more variation as a result of this because inevitably some centres will implement it quicker than others,” he said.
“So again measuring the difference between one-year survival in centres will be useful. So I imagine in a year from now we will have some data coming through telling us whether or not it is having an effect.”
<h3 class=”subheadMIstyles”>Ambitious</h3>
Prof Baldwin is confident the ambitious timelines and targets in the pathway are achievable.
“The initial knee-jerk response from radiologists, in particular, and some chest physicians, is that it is impossible. But what we have seen is that people have gone a long way to achieving it. It isn’t impossible. It is a real challenge though. There is no doubt about that. It does require commitment from physicians. And it isn’t particularly clinician-friendly in the sense that it requires a bit more of an immediate service.
“So one does need to have good clinicians who are prepared to cross-cover one another and make sure the service doesn’t get interrupted. And that does reduce the flexibility in your life as it were, but on the other hand these patients are terribly distressed and they go through an awful, awful experience and I think clinicians are very aware of that and want to improve the current situation.
“Lung cancer is a really big problem. Waiting times in lung cancer are a really big problem. Survival rates are appalling in lung cancer and we have evidence that this might improve survival.”
Prof Baldwin maintained that the pathway will bring the diagnosis of lung cancer forward substantially for 25 per cent of the patient population.
“That will have a measurable impact on one-year survival pretty quickly and that is one of the outcome measures we will be looking at when people implement that national clinical pathway, what the one-year survival is, because I think if we can show if this has a substantial effect on one-year survival then the Government in the UK will have very great difficulty going backwards on this. I think they will have difficulty now anyway, because what politician is going to say ‘Sorry, this pathway is too ambitious’. They are not going to say that easily. So it is here to stay in the UK.”










Leave a Reply
You must be logged in to post a comment.