At the end of last year, a national strategy for genetic and genomic medicine was finally launched. David Lynch examines the potential that the strategy offers to improve clinical care and research, as well as the likely challenges in implementation
“When I just think back at my time as a junior doctor, there are things done now that nobody would have believed back then,” according to Dr Colm Henry, HSE Chief Clinical Officer (CCO).
Dr Henry believes that genetic and genomic medicine has “revolutionised treatment”.
“When I was a junior doctor, I wouldn’t have dreamed about the way personalised medicine can be delivered now,” the HSE CCO told the Medical Independent (MI). “For example, cancer treatments were delivered in a very ‘one-size-fits-all’ manner. There were many conditions we thought were sporadic and random – we now know them to have a genetic foundation. It has revolutionised treatment.”
However, until now, much of this revolution has not been experienced in Ireland.
The new National Strategy for Accelerating Genetic and Genomic Medicine in Ireland, published in December 2022, aims to change this situation (see panel).
According to the HSE’s website, there is “room for improvement” in the medical genetics and genomics services offered in Ireland when compared to other European countries.
The strategy states: “To date, Ireland has made some progress in developing its genetic and genomic services, with pockets of excellence evident throughout the country. However, to fully realise the benefits of genetics and genomics, there is an urgent need to mainstream them so that they can become an integral part of our routine care delivery.”
Dr Henry said: “We wanted to make sure this country was better placed, not just in addressing existing structural and manpower problems, but [to] have a clear sense of direction of where we are going.”
In terms of recruitment in genetics, he added that Ireland wants to be a “place where we can attract the brightest and the best to work here”.
The Review of the Clinical Genetics Medical Workforce in Ireland 2019, produced by HSE National Doctors Training and Planning, found that only four clinical genetics specialists worked in the health service nationally at the time. Of these specialists, three were over the age of 55. This was against a backdrop of demand for at least 15 consultants. Irish patients were without access to genetic counselling and faced waiting times of between 15 and 18 months for priority cases and over two years for routine referrals.
In August last year, MI reported that the absence of a genomics strategy and multi-annual budget led to a “world-leading expert in genomics” declining the role of director of the planned national genetics and genomics medicine network.
However, Dr Henry is confident the new plans for the creation of a national office of genetics and a specific workforce plan will have a galvanising impact.
“We had difficulties recruiting before, it’s absolutely true,” he said, referring to MI’s August 2022 story.
“The reason is that we didn’t have a strategy for that person to implement and now, of course, not only do we have a strategy, we have €2.7 million from the Department of Health to kickstart some of this, including establishing the national office.”
He said the new positions in the national office will include a national director and clinical lead, a laboratory director, a bioinformatics director and support staff. “We need these staff to singularly focus on the priorities of year one, such as producing a workforce plan and also to look at current training, not just in genetics, but in other medical disciplines.”
“Strategies are very helpful in healthcare because a strategy gives you a sense of direction,” said Dr Henry. “We have a trauma strategy as you know, we have a cancer strategy, all of which have really improved the care in their particular domains…. We found that in the absence of a strategy, while we had areas of brilliance [in genetics], pockets of expertise, it was not tied together in a cohesive way. Also, in the absence of a strategy, you cannot guide multi-annual investment and address the areas of weakness in a very structured way.”
Recruitment
Dr Henry said six genetic counsellors and two consultant geneticists would be recruited prior to the creation of a new workforce plan. Beyond this, he has high hopes the strategy’s very existence will prove to be an attraction to doctors living abroad, while also impacting the training decisions of medical graduates.
“First thing is, we already have some excellent people… lots of clinicians working here would have brought their expertise back from training abroad,” Dr Henry said.
“But what I have found is when there are national strategies, such as cancer, it tends to attract staff. It tends to attract people home, it gives an incentive to people to study a particular area.
“If you are a medical graduate, for example, considering a career in the core discipline of medical genetics, or developing a specialist interest as part of another specialty, we find that [the existence of a strategy] tends to have a positive contagion effect on the healthcare system. It tends to have a snowball effect in interest in training and also attracting people home.”
On the impact of the national office, Dr Henry predicted there will be a high level of activity “in year one, and the office will drive it”. He said it will “become the engine of what happens in year two, three, four, and later”.
Also, the office will “advocate” and “compete for funding each year”.
Potential
MI has attended two major conferences on genetic and genomic medicine in recent years. At both events clinicians raised the lack of a national plan as a serious hurdle for progress. Now the strategy is published, how significant will it really prove?
“I think this is vitally important,” Prof Orla Hardiman, Clinical Lead, HSE National Clinical Programme for Neurology, and Consultant Neurologist at the National Neuroscience Centre of Ireland, Beaumont Hospital, Dublin, told MI.
Prof Hardiman described the new strategy as a “consensus document” generated “by all relevant stakeholders”. She added that it was a ‘roadmap’ that covers the perspectives of all involved, and such buy-in “will enable early implementation”.
“It is also very important that there is a very strong user perspective, which is essential,” she said, stating the “patient voice” was particularly important.
“The strategy also recognises the necessary interplay between clinical and research work in genomics, as the two are intimately linked.”
Prof Hardiman said the “next steps will now be very important”.
“As our understanding of disease evolves, it is very clear that genomics will inform much of our decision-making.”
She noted that in the past, the concept of genomics was confined to conditions for which there is a defined chromosomal abnormality or conditions with a clear inherited component that can be mapped across families. However, currently “genomics have the potential to inform decision-making across a wide range of disciplines”, she said.
“This is very much the case now in oncology, but it is also in evolution in all specialties as a precision medicine approach helps us to target individual pathogenic pathways, many of which are modified by genomic variation. And we also have early genomic therapies that are likely to expand over the coming years.”
Concerns
Prof Hardiman also highlighted potential challenges with implementation.
“The next step will be [to] ensure that there is adequate funding to implement a state-of-the-art programme,” said Prof Hardiman.
“I am concerned that the budget allocated for this may not be sufficient. A joint professorship in genomics [between University College Dublin and Trinity College Dublin] has been advertised to move the field forward, but the programme will require a very significant investment in infrastructure and personnel.”
She added that consideration would need to be given to whether the programme will be centralised, or whether each of the major teaching hospitals will be encouraged to develop a genomics department, with an appropriately funded cohort of clinical and laboratory personnel.
“As a neurologist with a specialty interest in the genomics of neurodegenerative diseases, my strong preference would be to have genetic counsellors linked to the service that I and my colleagues provide, rather than a centralised service with genetic counsellors that cater for the entire range of genetic disorders. However, this remains to be fully discussed.”
Prof Hardiman said discussion would also need to take place on the funding and access to a new genome biobank “and whether this should be funded out of the public purse, or in collaboration with private entities”.
“The latter consideration has been subject to much discussion over the years and from my understanding has not been fully resolved.”
Ethics
In May 2021, an online Royal Irish Academy conference focused on the lack of a national genomics policy and bioethical issues. Dr Oliver Feeney (PhD) is an Associate Researcher with the Centre of Bioethical Research and Analysis, Discipline of Philosophy, University of Galway, and was organiser of that event.
“Given the developments in genomic technology since the turn of the century, from whole genome sequencing to CRISPR gene editing, such a strategy is long overdue,” Dr Feeney told MI. Noting concerns over the “unregulated environment”, he said the strategy should not be considered a “finished product”, but something that has to continue to develop further in the coming years.
Dr Feeney said he believed “national coordination” would be pivotal for the strategy to prove successful. He said the strategy “emphasises public and patient involvement and genetic literacy to a great degree”.
“It also highlights the importance of ethical safeguards, particularly in terms of consent and data protection. These are all positive steps. But this is just the beginning of the ethical discussions that need to be much more developed and elaborated in the forthcoming months.”
Dr Feeney said “the strategy touches upon some ethical issues, and gestures towards the importance of ethics in general, but little more”.
“A number of issues face genomics as opposed to earlier forms of genetic research and other non-genomic forms of research,” he added. “For one thing, the reality or rhetoric of genuine informed consent with the individual keeping control over their data may be increasingly strained in a context where research is large-scale, international, and where secondary use of such data may elude such control.”
He pointed out “transparency is needed” regarding promises in the strategy to be able to refuse consent in the future and the right to withdraw your data from research.
The strategy notes that guidance on consent for genetic and genomic clinical and research purposes will be developed in line with the HSE national consent policy and the national consent for research policy, which is currently in development.
“The clinical application of whole-genome sequencing can also potentially identify variants in genes for unknown functions or where uncertainty exists over the relation to disease,” he said. “Such incidental findings, which are unrelated to the goals of the test or study, and are discovered unintentionally, raise questions on what to do with such discoveries in a clinical context.”
Dr Feeney added that other ethical questions arise including those “regarding the risk of genetic discrimination and stigmatisation”; how it will affect persons with disabilities that may have a genetic component; and how this information may contribute to increased abilities in predictive decision-making in the context of assisted reproduction.
“These are only the tip of the ethical or bioethical issues involved. Minister for Health Stephen Donnelly, in his foreword to the strategy, said that it ‘lays out a wider vision for Ireland’s future genetic and genomic service’. Insofar as it does, this vision needs a stronger bioethical lens than currently is the case.”
He noted that there has been “some movement” in terms of national ethics or bioethics infrastructure (“For instance, the national office for research ethics committees has national coordination at its core”). However, Dr Feeney argued that “in terms of broader bioethical questions, we are still in a largely ad hoc situation”.
As our understanding of disease evolves,
it is very clear
that genomics will inform much of
our decision-making
Literacy
Improving genetic literacy is a major aim of the strategy, Dr Henry told MI, not only among the general public, “but also among healthcare workers.”
For doctors, the aim is to raise “awareness of genomic medicine for all medicine disciplines, not just those training to
be geneticists”.
“I don’t want to be critical, there is a high level of awareness among medical graduates who have a very high education from our medical schools, about the power of this,” said Dr Henry. “But we want to make sure that we avoid what somebody called the ‘ghettoisation of genetics’ into a core specialty. There needs to be a heightened sense of awareness of its power and its role and application across all disciplines, not just the core discipline of genetics.”
Is there sufficient information technology (IT) infrastructure underpinning the health service to carry this strategy?
“Yes, of course, that is absolutely huge, no doubt about it,” Dr Henry replied. He said that while IT is not something the strategy is focused on over the first year, “once we get to a higher level” it will be crucial.
“The creation of an individual health identifier will produce more efficient and safer care not just for genetics, but right across our health system. It has to a priority when you consider not just the safety issue, the information issue, but also the waste issue that goes along with not having a single identifier for patients that can be used at all points of presentation in the healthcare system.”
Immediate priorities in the strategy
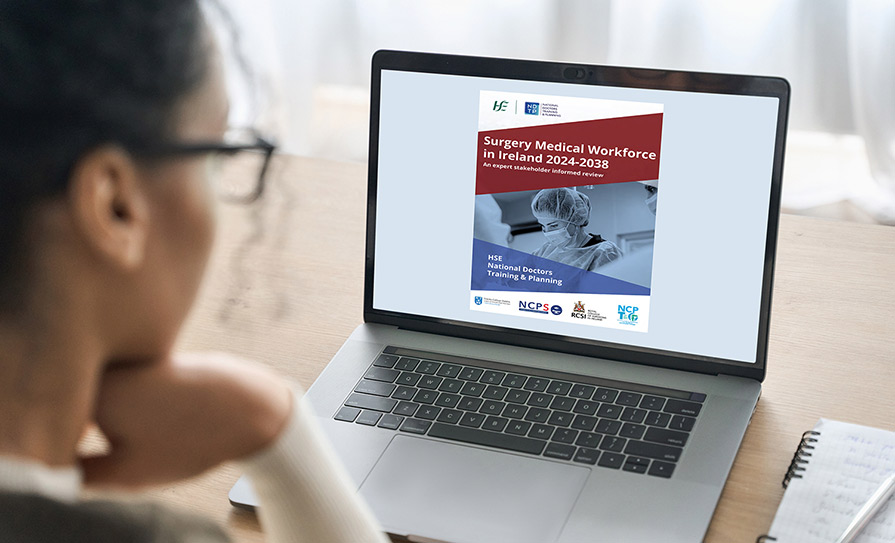
The National Strategy for Accelerating Genetic and Genomic Medicine in Ireland was produced by a steering group of experts chaired by Dr Mark Bale, former Genomics Advisor to the UK Department of Health.
The strategy addresses issues, such as shortages of trained genetic specialists; knowledge gaps in the clinical workforce; the lack of genetic/genomic literacy across healthcare professions and the public; and the policies needed to make the service “ethical and inclusive”. It also proposes the creation of a centralised national body with responsibility for the oversight and coordination of genetic services.
The plan outlines a number of clear commitments that will begin during the next 12 months. The highest profile of these include:
- A national office for genetics and genomics will be established in 2023 under the governance of the HSE and will provide oversight and a standardised approach to the delivery of the genetics and genomics service.
- A national genetics and genomics workforce plan will be developed in 2023 to support the recruitment, retention, education, and career development of the current and future genetics and genomics workforce.
- “Equitable, timely, and evidence-based availability of genetic and genomic tests and technologies in clinical practice will be improved through a coordinated and standardised national approach,” according to the strategy. The development of a national test directory will commence in 2023.
- A national centre of excellence
in genomic testing and bioinformatics will be established as a single entity, which will sit under the governance of the HSE.