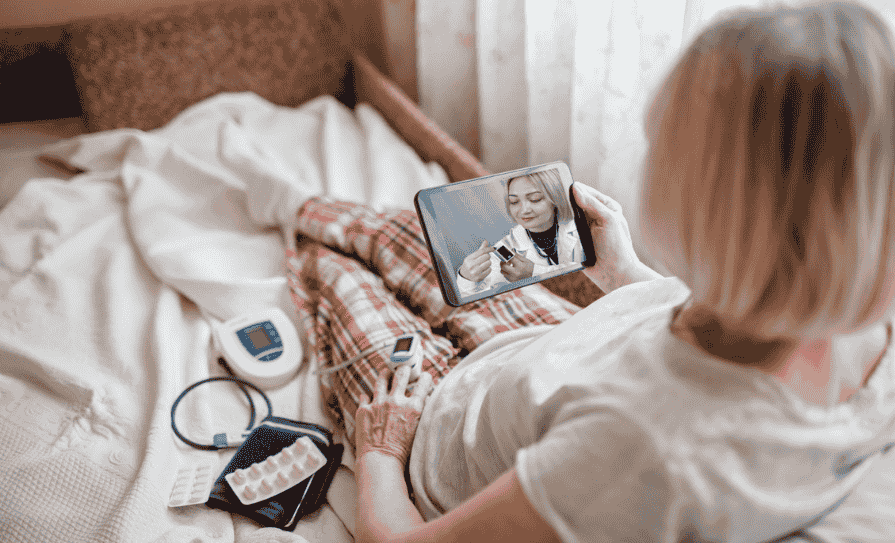
A new digital initiative is being launched for cardiology and respiratory patients at St Vincent’s University Hospital, Dublin, and University Hospital Limerick. Virtual wards are expected to offer a safe and efficient alternative to hospital stays and support patients who prefer to receive expert hospital care through monitoring and treatment in their own homes. The virtual ward service may be offered to appropriate hospital inpatients with a respiratory or cardiac condition that are medically stable, but require ongoing monitoring and care prior to formal discharge.
HSE Chief Clinical Information Officer Prof Richard Greene noted that virtual wards are “a new health innovation that has emerged internationally”. He also said: “Central to the National Virtual Wards Programme is the empowerment of patients to be active partners in managing their health and wellbeing. Patients remain under the care of the consultant-led team that provided their care in the hospital and will have a dedicated team monitoring their care 24/7, while they are in the comfort of their own home.”
Healthcare teams will work with patients, and their families or carers if appropriate, to assess whether individuals might be suitable to be treated through the virtual ward service. A member of the clinical team will explain how the service works and why they think it might be a suitable option, and will also ensure patients/carers receive adequate education and training regarding any equipment they will be given. Once a patient is transferred to the virtual ward service, they remain under the care of the consultant team that provided their care in the hospital.
A personalised care plan will be agreed between the patient, their family/carer, and consultant-led care team, and they will establish the best ways to make contact, as well as what to do if the patient feels unwell. Care will continue to be reviewed 24 hours per day, seven days a week by their consultant-led care team. The virtual ward team will be automatically alerted by the monitoring technology if the patient’s readings worsen, or if they are not responding to treatment as expected. Following completion of the patients’ treatment and care, they will be discharged by the consultant-led care team from the virtual ward.
Maureen Gilbert, patient representative on the Virtual Ward Steering Group, described the virtual wards initiative as “a really positive development”, and said it will “offer great potential for patients and their empowerment”.
She added: “Virtual wards can support enhanced recovery, and there’s more quality one-to-one communication between patients and their care team. Research shows that patients who recover at home experience less of the stress and anxiety that can sometimes be associated with a hospital stay. There are lots of other benefits too – lower risk of hospital-acquired infection and loss of muscle strength. People who join virtual wards can be more active partners in their own healthcare and they are less likely to need another inpatient hospital stay in the near future.”
The national Virtual Wards programme is a collaborative initiative bringing together stakeholders from across the health service including eHealth Ireland, the National Clinical Programme Respiratory, the National Heart Programme, St Vincent’s University Hospital, and University Hospital Limerick.









Leave a Reply
You must be logged in to post a comment.