Reference: March-April 2024 | Issue 2 | Volume 17 | Page 34
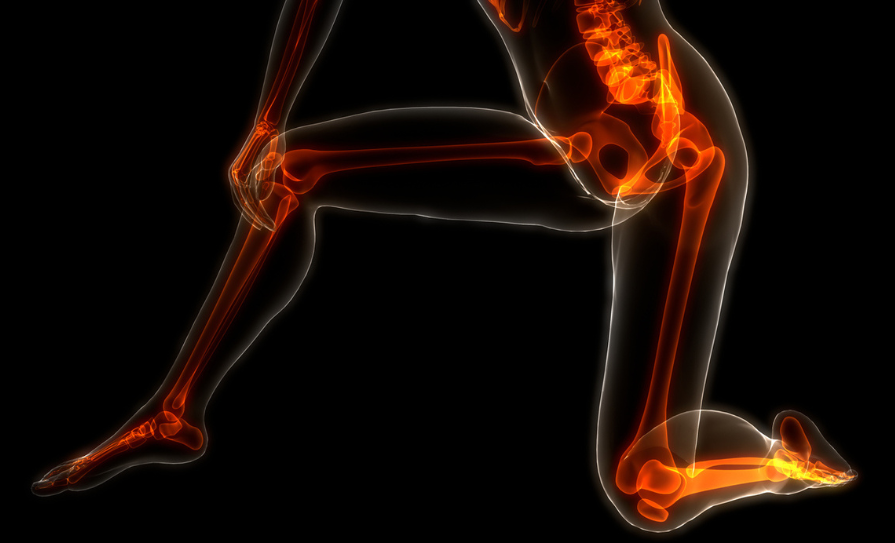
Neuropathic pain, or neuropathy, is a multifaceted condition characterised by pain as a result of damage or illness affecting the somatosensory nervous system. It encompasses the peripheral and central nervous systems, and is often caused by various aetiologies such as diabetes, infections, trauma, autoimmune disorders, or metabolic disturbances. Most often the damage occurs within the peripheral nervous system. However, conditions like cerebrovascular accident (CVA) can also lead to neuropathic symptoms. Neuropathy is a leading cause of chronic pain, which persists for three months or longer. Around 8 per cent of individuals with chronic pain experience some variation of neuropathy. Globally, the condition affects millions of people, with prevalence rates varying across different populations and age groups. An estimated 10 per cent of the global population has neuropathic pain.1,2
Neuropathic pain
Manifestations of neuropathy depend on the specific nerves involved. When sensory nerves are affected, they can lead to symptoms of numbness, weakness, and sharp or burning pain which may exacerbate without early intervention. Impairment to nerves responsible for touch, vibration, and temperature perception can lead to tingling, numbness, or the sensation of wearing a glove-like covering on the hands or feet. Damage to motor nerves that control stability and movement can cause a lack of coordination, weakness, or cramping. Damage to autonomic nerves, regulating internal organ function, can result in reduced saliva, tears, perspiration, or dysfunction within other organs or glands.1,2
The sensation of neuropathic pain is unique. The area of pain may be widespread or limited to a single or several nerves.Typical causes of neuropathic pain include nerve pain from spinal disorders; post-amputation pain; chronic pain from other nerve trauma or injury; complex regional pain syndrome; vascular disease; drugs such as chemotherapy; and neuropathies that may occur after a viral infection or from metabolic disorders like diabetes.2 Neuropathic pain is common in cancer patients, in which the perceived pain often has mixed neuropathic and nociceptive components.5
Pain of neuropathic origin includes neuralgia, such as the facial pain syndrome trigeminal neuralgia. Another pain of neuropathic origin is neuritis, caused by inflammation of a nerve or group of nerves, and may be accompanied by fever and swelling.2
Peripheral neuropathy
Painful peripheral neuropathy is a common neurological disorder characterised by numbness, weakness, tingling, and pain, often starting in the hands or feet. More than two out of every 100 people are estimated to have peripheral neuropathy, and the incidence rises to eight in every 100 for people aged 55 or older. When a single nerve is impacted, it is called mononeuropathy. When multiple nerves are affected, it is called mononeuritis multiplex. If it affects both sides of the body, it is termed polyneuropathy. This condition can be widespread or confined to a specific area, known as focal peripheral neuropathy.2 Peripheral neuropathies stem from a variety of origins, including metabolic, systemic, and toxic causes. In some cases, a direct cause may not be apparent. Peripheral neuropathies typically emerge gradually over months-to-years, although some may progress rapidly. They vary widely in severity and symptoms, impacting motor, sensory, and autonomic nerve fibres.6
Complications of peripheral neuropathies include pain, altered sensation, muscle atrophy, and weakness. Diabetic peripheral neuropathy complications include foot ulcers which can lead to gangrenous digits and limbs, sometimes progressing to amputation.6
Clinical presentation
The clinical presentation of neuropathic pain is diverse, as it depends on the nerves affected and underlying conditions. Among the signs and symptoms of neuropathic pain are allodynia – a pain due to a stimulus that does not normally provoke pain; hyperalgesia – an increase in the perception of pain generated by a stimulus that causes pain; dysesthesia – an unpleasant feeling, which is not actually painful; and paraesthesia – an unusual sensation, such as pins and needles or a burning sensation.2
Patients may report symptoms including tingling, burning, shooting pain, numbness, and heightened sensitivity to touch. The pain may be described as feeling like a stabbing, burning, electric shock, or a freezing sensation. It may worsen at night. Some people may experience temporary numbness, tingling, and pricking sensations, sensitivity to touch, or muscle weakness. Others may experience more extreme symptoms, such as burning pain, muscle wasting, or even paralysis. Neuropathic pain is typically chronic, debilitating, and challenging to manage, and can significantly impact an individual’s quality-of-life.1
Many neuropathic pain patients experience other symptoms such as alterations in mood leading to depression, anxiety, sleep disorder, neurocognitive impairment, generalised malaise, and other poorly described complaints.5 Neuropathy is more prevalent among women, and more frequently reported by manual workers, as well as among people from rural areas.3
Diagnosis
Diagnosing neuropathic pain requires a comprehensive evaluation that includes a holistic patient history, clinical examination, and often, specialised tests. Assessing the specific characteristics of pain, its distribution, and understanding that associated neurological deficits play an important role in differentiating neuropathic pain from other pain types are essential.6,7
Patient history: A detailed medical history is the initial step in diagnosing neuropathic pain. Key elements include identifying the onset, duration, and progression of symptoms. Understanding the quality and characteristics of pain, eg, burning, shooting, tingling, and factors that exacerbate or alleviate it helps to differentiate neuropathic pain from other types. Exploring associated comorbidities, injuries, surgeries, medications, and family history of neurological disorders aids in narrowing down potential causes. Past medical history should inquire about toxic exposures, present and past medications, trauma, dietary and nutritional deficiencies, and alcohol use.1,2,6
Clinical examination: A thorough neurological examination includes assessing sensory function, motor strength, reflexes, and the presence of any neurological deficits. Specific tests such as assessing sensation to light touch, pinprick, temperature, and proprioception help to localise and characterise nerve involvement.1,2,6
Specialised tests: Specific investigations may assist in confirming neuropathic pain and identifying underlying causes.
Electrodiagnostic studies: Nerve conduction studies and electromyography evaluate nerve function and detect abnormalities in nerve transmission or muscle response.6
Imaging studies: Magnetic resonance imaging (MRI), computed tomography (CT) scans, or nerve imaging techniques may reveal structural abnormalities, compressions, or lesions affecting nerves or the central nervous system.6
Laboratory tests: Blood tests can screen for conditions like diabetes, vitamin deficiencies, infections, autoimmune disorders, or metabolic disturbances that can lead to neuropathy.1,6. Necessary laboratory tests for peripheral neuropathy include a full blood count, erythrocyte sedimentation rate, comprehensive metabolic panel (blood glucose, HbA1c, renal function, liver function), thyroid function tests, vitamin B12 levels, and serum protein immunofixation.8
Clinicians often refer to established criteria like the Douleur Neuropathique 4 questionnaire or Leeds Assessment of Neuropathic Symptoms and Signs scale. These tools help quantify and classify neuropathic pain based on characteristic symptoms and clinical signs.9
Differential diagnosis: Distinguishing neuropathic pain from other pain types, such as nociceptive or inflammatory pain, is important. Nociceptive pain typically results from tissue damage, while neuropathic pain arises from nerve dysfunction. Patients may experience a combination of both, necessitating careful evaluation to guide appropriate treatment.1,6
Collaboration among specialists like neurologists, pain management specialists, and primary care clinicians is important for accurate diagnosis and management. Regular follow-ups allow for monitoring symptom progression, treatment efficacy, and necessary adjustments in the management plan.1,6
Treatment strategies
Managing neuropathic pain is a clinical challenge due to its complexity and varied aetiologies. A multimodal approach combining pharmacological and non-pharmacological interventions is often required. Neuropathic pain, particularly in those with small-fibre neuropathies, does not typically respond to simple analgesics. Medications such as anticonvulsants, antidepressants, topical agents, and opioid analgesics are commonly used. Interventions like physical therapy, transcutaneous electrical nerve stimulation (TENS), nerve blocks, and psychological therapies contribute to holistic pain management.1,6
The most recent systematic review and meta-analysis on drug efficacy for neuropathic pain included a total of 229 studies.4 The Special Interest Group on Neuropathic Pain (NeuPSIG) identified gabapentinoids, tricyclic antidepressants, and selective serotonin–norepinephrine reuptake inhibitors as first-line drugs for neuropathic pain. Lidocaine, capsaicin, and tramadol are suggested as the second-line treatments, while strong opioids such as morphine, oxycodone and botulinum toxin-A are included as third-line treatments for peripheral neuropathic pain.4
Treatment of peripheral neuropathies should focus on the treatment of the underlying disease process, eg, glucose control in diabetic neuropathy and alcohol cessation in alcoholic neuropathy. Nutritional deficiencies can be treated with supplementation of depleted vitamins or minerals and promotion of a healthy balanced diet. Unfortunately, not all peripheral neuropathies are reversible. Physical therapy and occupational therapy can be initiated to aid in the improvement of a patient’s overall strength and function. Chronic inflammatory demyelinating neuropathy is treated using corticosteroids initially, but can also be treated using intravenous immunoglobulin, plasma exchange, and some immunosuppressant drugs.6,7
Emerging therapies and research
Neuropathic pain poses a significant medical challenge due to the limited effectiveness or side-effects of current treatments, therefore, new therapeutic interventions are important. Several compounds targeting new pain pathways are in early development, with only a handful of clinical trials suggesting their potential in neuropathic pain management. NaV1.7 antagonists and angiotensin type II inhibitors show promise. Established drugs like botulinum toxin A and the anti-epileptic oxcarbazepine have demonstrated efficacy in treating peripheral neuropathic pain. Emerging non-drug therapies, including non-invasive brain neurostimulation techniques like repetitive transcranial magnetic stimulation and transcranial direct-current stimulation, also show encouraging results in managing neuropathic pain. Other recent advancements in neuropathy management include innovative approaches such as neuromodulation techniques, gene therapy, and targeted drug delivery systems. Ongoing research explores the pathophysiology of neuropathy to find novel therapeutic targets and personalised treatment options for better pain control and improved patient outcomes.10
Support
In Europe, one-in-five people are living with chronic pain. In Ireland, the figure is higher, with one-in-three people affected, and one-in-five people living with pain for 10 years or more.11
Chronic Pain Ireland is the national organisation providing information and support services to people living with chronic pain in Ireland. They can be contacted via email or helpline at 01 8047567.
References
- Cavalli E, Mammana S, Nicoletti F, Bramanti P, Mazzon E. The neuropathic pain: An overview of the current treatment and future therapeutic approaches. Int J Immunopathol Pharmacol. 2019;33:2058738419838383.
- Christelis N. Neuropathy, Neuropathic Pain, and Painful Peripheral Neuropathy. International Neuromodulation Society: Vancouver; 2017. Available at: www.neuromodulation.com/fact_sheet_painful_peripheral_neuropath.
- Van Hecke O, Austin SK, Khan RA, Smith BH, Torrance N. Neuropathic pain in the general population: A systematic review of epidemiological studies Pain. 2014;155(4):654-662.
- Finnerup NB, Attal N, Haroutounian S, et al. Pharmacotherapy for neuropathic pain in adults: A systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162-173.
- Van Velzen M, Dahan A, Niesters M. Neuropathic Pain: Challenges and Opportunities. Front Pain Res (Lausanne). 2020;1:1.
- Hammi C, Yeung B. Neuropathy. In StatPearls Publishing: Treasure Island; 2023. Available at: www.ncbi.nlm.nih.gov/books/NBK542220/.
- Saperstein DS, Katz JS, Amato AA, Barohn RJ. Clinical spectrum of chronic acquired demyelinating polyneuropathies. Muscle Nerve. 2001;24(3):311-324.
- Lehmann HC, Wunderlich G, Fink GR, Sommer C. Diagnosis of peripheral neuropathy. Neurol Res Pract. 2020;2:20.
- Abolkhair AB, El-Kabbani AO, Al-Mulhem A, et al. Psychometric and accuracy comparison of three commonly used questionnaires for the diagnosis of neuropathic pain. Saudi J Anaesth. 2021;15(4):409-418.
- Bouhassira D, Attal N. Emerging therapies for neuropathic pain: New molecules or new indications for old treatments?. Pain. 2018;159(3):576-582.
- Murphy P. What is chronic pain? Chronic Pain Ireland: Dublin; 2023. Available at: www.chronicpain.ie/what-is-chronic-pain/.












Leave a Reply
You must be logged in to post a comment.