Ireland’s health system is constantly in the news. We hear about trolley numbers and waiting lists, screening programmes and adverse events, court settlements and fitness to practise hearings, and endless other accounts of the ways that things go wrong. From time-to-time, a counter-narrative is permitted to emerge, emphasising all that is right about Irish healthcare, providing realistic and often positive comparisons with other countries, and pointing to the parts of our system that work well.
General practice is usually high on the list of things that work well. Indeed, primary care is often cited as the only part of the Irish health system that actually functions at all, despite its resource challenges and a general under-appreciation of its role. While I do not agree that all the rest of the health system is dysfunctional, it is hard to deny that the benefits delivered by primary care are still under-valued in Ireland compared to other countries and compared to other parts of the health system. This perception needs to change.
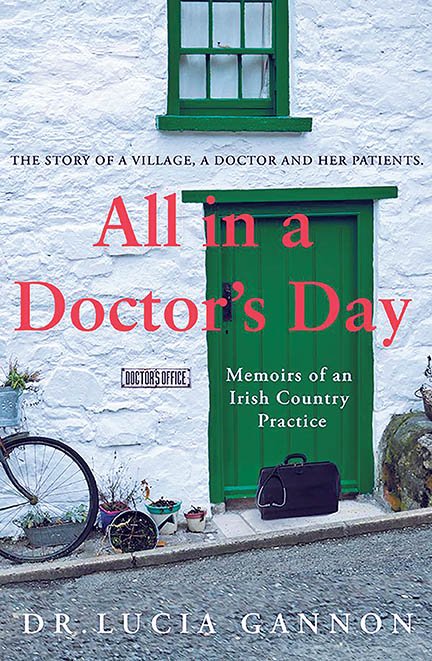
Citing statistics, such as numbers of patients seen or services offered, is one important way of doing this, but the language of statistics does not appeal to everyone and statistics cannot provide a granular feel for the challenges and rewards of general practice. One of the best ways to remedy this is, perhaps, for doctors to articulate what it is like to work as a GP in Ireland today: The problems, the solutions, the outcomes. And this is precisely what Dr Lucia Gannon does in her fascinating new book, All in a Doctor’s Day: Memoirs of an Irish Country Practice (Gill Books, 2019), which is “the story of a village, a doctor and her patients”.
Gannon, a GP in Killenaule, Co Tipperary, qualified in medicine from NUI Galway (then UCG) in 1986 and completed her GP training in the UK. She worked in various posts around Ireland before arriving in Killenaule, where she now lives, working alongside her husband, who is also a GP in the village.
The story of Gannon’s peripatetic training will be familiar to many readers from their own lives, along with her deepening involvement in education and training over the years: Gannon was a GP Clinical Tutor for the University of Limerick Graduate Entry Medical School (GEMS) from 2010 to 2018, and is currently an Assistant Programme Director with the South-East GP Training Scheme. She has special interests in mental health, infant nutrition and medical education, and somehow also finds time to contribute to this newspaper (although I should add that I do not know her at all).
And now Gannon has written a truly engrossing book looking not only at her patients’ illnesses and consultations, but also at what it is like to be a GP in rural Ireland today. She starts by outlining her own training path into general practice and the process of setting up a surgery in Killenaule. She goes on to present a range of case vignettes with a strong emphasis on the hugely varied issues that bring people into GP surgeries and the similarly varied responses required of her. These encounters constitute one of the two key features of this invaluable book, the other being Gannon’s reflections on her own life and work, especially in the context of her growing family and her complex, privileged position as a doctor in the village.
Throughout the text, Gannon places huge emphasis on doctor-patient interaction and especially the necessity for kindness. “Medicine”, she writes, “has limits, but kindness does not”. While most of us are only too well aware of the limits of medicine, it is easy to fall into the trap of thinking that there are limits to kindness too. But as Gannon points out — and, more compellingly, demonstrates — there are no absolute limits to kindness; while we all experience kindness-fatigue at times, this can be fixed by taking time to recharge the batteries.
Gannon also speaks about the complex realities of living and working as a GP in a relatively small community, where family lives overlap and therapeutic relationships often last a lifetime. This presents both opportunities and challenges, so setting the right tone with patients is essential. Gannon does a good job drawing out the complexities of this, and demonstrates how setting limits is both necessary and (in a sense) impossible in such an intensely local setting: One must certainly regulate access but, in the end, the door always stays a little bit open.
This is a book about the realities of clinical practice, how to be a good doctor, and how to live in a small community as their physician. All told, it is a subtle, powerful memoir, written in an easy-to-read style that belies the seriousness of Gannon’s intent.
William Osler (1849-1919), Canadian physician, founding professor of Johns Hopkins, and doctor-writer extraordinaire, advised doctors to “observe, record, tabulate, communicate. Use your five senses. Learn to see, learn to hear, learn to feel, learn to smell, and know that by practice alone, you can become expert.” Gannon’s book achieves all of these goals: Closely observing herself and her patients, faithfully recording her experiences, and communicating with a fluency that makes All in a Doctor’s Day one of the most significant books about Irish medicine since the turn of the century.
Prof Brendan Kelly is Professor of
Psychiatry at Trinity College Dublin and author of ‘The Doctor Who Sat For A
Year’
(Gill, 2019).






Leave a Reply
You must be logged in to post a comment.