Health inequalities in Traveller communities have worsened during the Covid-19 pandemic, yet there is still no plan to address these disparities. Niamh Quinlan reports.
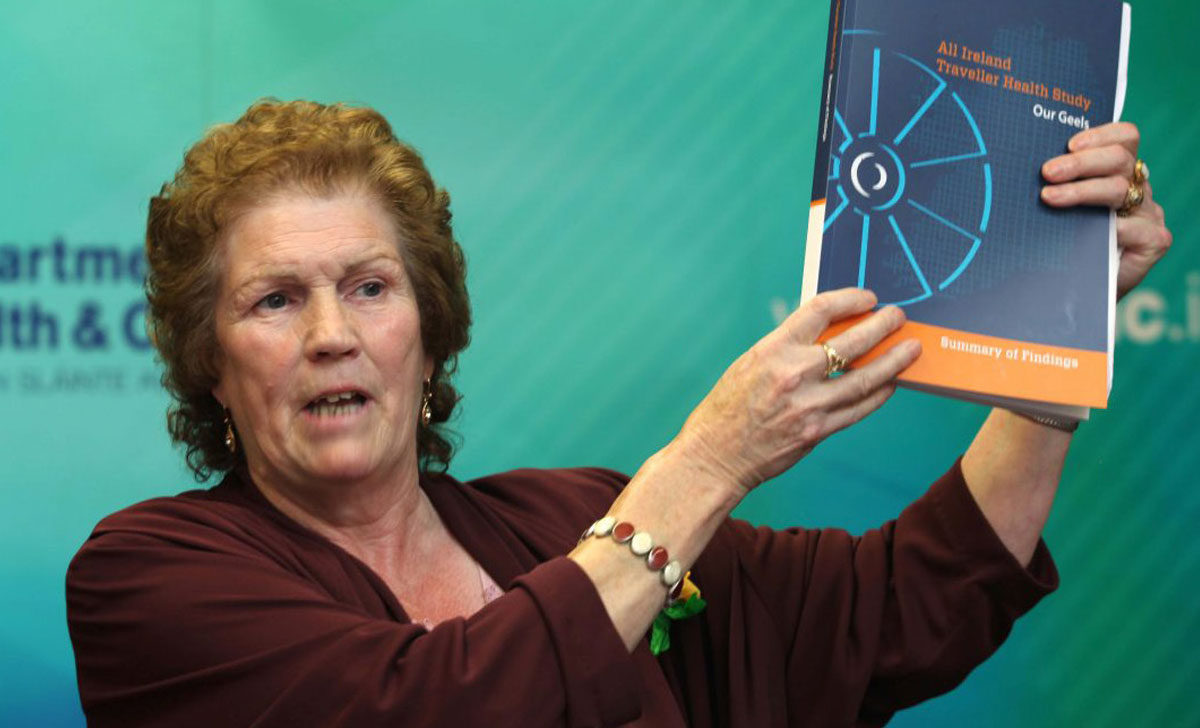
In 2010, the All Ireland Traveller Health Study (AITHS) revealed the serious health inequalities faced by the Traveller community. Since then, the development and implementation of a plan to tackle these inequalities has been promised.
In each HSE national service plan since 2019, one of the Executive’s priorities and actions has been to “finalise” a plan in line with the National Traveller and Roma Inclusion Strategy 2017-2021 (NTRIS). The strategy is a cross-departmental initiative tasked with improving the lives of Traveller and Roma communities in Ireland.
In the foreword to the NTRIS, the then Minister of State with special responsibility for Equality, Immigration, and Integration, David Stanton, said the strategy was intended to reinvigorate “efforts by the State to ensure that Travellers and Roma interact fully with the public health sector in order to address some of the underlying health-related challenges facing those communities”.
A key recommendation in the NTRIS was for the HSE to develop and implement “a detailed action plan” based on the findings of the AITHS, “to continue to address the specific health needs of Travellers, using a social determinants approach”.
However, the HSE and Department of Health have not confirmed a date for the publication of a National Traveller Health Action Plan (NTHAP).
‘Frustration’
The uncertainty surrounding the NTHAP has left many within the Traveller community and those working with Traveller communities frustrated.
A HSE spokesperson told the Medical Independent (MI) the finalisation and publication of the plan remained a priority.
A draft plan, which was circulated by the HSE in March 2019, was found by stakeholders to be inadequate in its provisions. As a result, the Executive committed to redrafting the plan.
“We’ve been 12 years, basically, waiting for it [NTHAP],” Policy Analyst and Traveller Health Researcher at Pavee Point, Ms Lynsey Kavanagh, told MI.
Ms Kavanagh said Pavee Point was urging the Department of Health and the HSE to give an indicative date for the publication, including a clear implementation plan and associated ringfenced budget for Traveller health. “It doesn’t have to be tomorrow. It doesn’t have to be next week. But we want an indicative date for the publication.”
“And Traveller organisations and Travellers on the ground are rightfully frustrated… [they] really bought into the process that this could potentially have a significant impact on Traveller health and yet we’re sitting in 2022 being told there’s no date,” said Ms Kavanagh. “And from our perspective, it’s this political football that’s being kicked around.”
A spokesperson for the Department told this newspaper: “The Department acknowledges the frustration of Traveller organisations arising from the delay in publishing the plan. The publication and implementation of the plan is a priority for the Department and the HSE in 2022.”
Regarding the implementation of the NTHAP, Ms Kavanagh said Pavee Point was “on public record saying that without indicators, without resources, without budgets and also not reflecting the consultation report, we can’t endorse it and we can’t support it”.
The Department of Health and the HSE are in discussions to identify the resources required to implement the NTHAP, according to the Department spokesperson.
“The Department of Health is fully committed to providing the leadership and resources to ensure the implementation of the plan by the HSE, once agreed,” the spokesperson said.
A spokesperson for the HSE told MI: “Once published, actions within the NTHAP will be prioritised and submitted to the Department of Health for funding in line with the 2023 estimates process.” A budget “to strengthen health supports for Travellers and initiate implementation of the NTHAP” has been ringfenced.
In 2021, the Department also provided €274,449 to expand Traveller health units (THU). A response to a parliamentary question in October 2021 stated that the Department had set aside €548,898 in 2022 for THU expansion.
The Department added that, upon implementation, “the plan will reflect the lessons from the public health response to Covid-19.”
Covid collaborations
The collaborations between Traveller rights organisations and public health during the Covid-19 pandemic must continue, according to Public Health Lead for Social Inclusion and Vulnerable Groups Dr Margaret Fitzgerald.
“Let’s not break that link now,” Dr Fitzgerald told MI. “Let’s keep going with the Traveller health…. Because it’s not just Covid. Now we’re looking at all the other health challenges Travellers have, with cancer, chronic diseases, early mortality… mental health, addiction.”
Dr Fitzgerald added that she also hopes collaborations during the pandemic helped Traveller communities to trust public health. “I think that wider trust in the health system is definitely going to help the [other] health issues for Travellers.”
‘A perfect storm’ – Traveller health inequalities aggravated by Covid
Covid-19 and its accompanying restrictions, combined with poor facilities and difficulties in carrying out isolation and social distancing on Traveller halting sites, meant health defences in the community against the virus were poor.
Policy Analyst and Traveller Health Researcher at Pavee Point, Ms Lynsey Kavanagh, described the pandemic as “a perfect storm, in terms of exacerbating those health inequalities”.
“What you had was Travellers who were living in really severely over cramped, overcrowded accommodation, without really the capacity to self-isolate, to be able to follow the basic hygiene that everybody was supposed to be able to do,” said Ms Kavanagh. “We were extremely concerned.”
While handwashing was a primary defence against the virus, many Travellers were without taps and running water. Traveller Primary Health Care Project (TPHCP) Assistant Coordinator, Ms Mary Brigid Collins, told the Medical Independent: “If you’ve only one tap between two trailers… that was quite difficult for them.”
The move to online interactions, including virtual health consultations, was also a challenge faced by Travellers. “If you have no internet connection, if you don’t have literacy, it was very difficult to go online,” according to Ms Collins. “And I think, with the huge health inequalities that we’re actually facing at the minute, that’s going to be difficult if [virtual healthcare is further embedded] in the future.”
According to the 2016 Census, 59.9 per cent of Travellers did not have access to the internet, compared to 18.3 per cent of the non-Traveller population. An estimated half of Travellers also struggled with literacy, according to The All Ireland Traveller Health Survey (AITHS) published in 2010. This has implications in terms reading medication and prescription information.
The AITHS revealed huge inequalities faced by the community compared to the general population: Traveller women and men had a life expectancy of 11.5 years and 15.1 years less than the general population, respectively; 12 per cent of Travellers had bronchitis compared to 3 per cent of the non-Traveller population; and 12.5 per cent had asthma compared to 6 per cent of the non-Traveller population.
Mental health was already a huge issue within the Traveller community before the pandemic. According to the AITHS, the rate of suicide among Traveller men was nearly seven times higher than the average population, with Pavee Point estimating 11 per cent of Traveller deaths were caused by suicide.
Addiction issues, already prevalent in the community were also exacerbated by lockdown conditions. Over 66.3 per cent of Travellers in the Republic said drugs were a problem within their own community, according to the AITHS. “That was in 2010,” said Ms Collins. “We know from the work that we do on the ground, and during the pandemic, that it has actually got much worse.”
Cancer support for the Traveller community
The Marie Keating Foundation (MKF) has worked with the Pavee Point Traveller and Roma Centre to inform Travellers about cancer issues.
Together with Pavee Point, the MKF provided “accessible, timely, culturally appropriate cancer awareness, and prevention information sessions” on some of the most common cancers which affect the Traveller community in Ireland.
Director of Nursing Services at the Marie Keating Foundation, Ms Helen Forristal, said the MKF had continued to communicate with the Traveller primary healthcare project team at Pavee Point, despite the change of priorities due to the pandemic. The two organisations worked together over the last year to develop an educational ‘social inclusion hub’ on the MKF website. “Within that, we started conversations around targeting cancer awareness,” Ms Forristal told the Medical Independent.
The Foundation also deployed bespoke cancer information resources to promote early detection and further awareness.
One MKF workshop informed Traveller primary healthcare workers about the process of cervical screening and detection of ovarian cancer.
“I feel that we empowered the Traveller women to take some positive actions,” said Ms Forristal, “for the benefit of their own health and for their own wellbeing.”
She said the Foundation also spoke to a group of men about prostate cancer: “With prostate cancer, particularly, there may be no signs or symptoms and there may be no reason, even pre- Covid, to consider going to the doctor to talk about it.” Men were encouraged to look for a history of prostate cancer and speak to doctors or their primary healthcare worker about prostate specific antigen blood tests.
According to the AITHS, Traveller women attended breast and cervical cancer screens at almost twice the rate of non-Traveller women.
The activity of screening services was severely curtailed during the pandemic. “We now have to work on that again and get it up and running,” said Ms Collins.
“We didn’t leave them alone, and I think that was very important,” she said. “We tried to make sure our Travellers felt that we would not walk away from them, that we would listen to them, that if we heard there was a major outbreak or there was a major upset, we would take it on board and do something.”
Since the beginning of the pandemic, the HSE National Social Inclusion Office (NSIO) understood that vulnerable groups “could be greatly affected” by the virus, according to Dr Fitzgerald.
“I focused on bridging the gap between our national and our local social inclusion teams, and between national and regional public health departments,” Dr Fitzgerald said. This included engagement and coordination with the HSE, other Governmental departments, and NGOs, such as Pavee Point.
A Covid-19 Traveller outbreak control team was established in September 2020, and continued until May 2021 to monitor and control breakouts in the Traveller community. Safetynet, a medical charity which provides health services to vulnerable groups, developed a Covid cluster rapid response team, mainly for the greater Dublin area, which was partly funded by the HSE.
In association with local authorities, the NSIO carried out risk assessments on Traveller halting sites. “I think the Traveller community found that very, very useful,” said Dr Fitzgerald. “Because some practical improvements did take place [with regard to] hot running water, electricity, washing machines, these sorts of practical things.” Cleaning and disinfecting sites, waste removal, and additional mobile homes and demountable accommodation to facilitate isolation and alleviate overcrowding were also provided.
The effectiveness of risk assessments was referenced in the Report on the National Traveller Covid-19 Accommodation Preparedness Checklist, published in July 2021. This report said: “This collaboration between [Department of Housing, Local Government and Heritage, local authorities, Traveller Health Units, HSE Social Inclusion, HSE Public Health, and primary healthcare for Traveller projects] has had a positive effect on the health outcomes of Travellers. This relationship should be encouraged and maintained beyond Covid-19.”
Travellers were also identified as a priority group for vaccinations.
“When vaccinations came in, we moved away from putting a huge emphasis on outbreak detection and control,” said Dr Fitzgerald. “And we put more emphasis into getting the vaccine out to the Travellers, improving the access and also… delivering the information to them in a way that they could engage with, because there was a lot of hesitancy.”
According to Dr Fitzgerald, much of the information about Government messages and measures was adapted “into a format that Traveller groups could relate to and understand and use their own WhatsApp and Facebook and their own ways of communication”. These also included resource pages on the HSE website and pop-up clinics around the country.
In terms of managing and responding to outbreaks of Covid-19 in Traveller communities, the HSE prioritised “working with THUs and non-Government organisation partners to enhance information and awareness about hygiene, Government measures on social distancing, restricted movements etc”.
According to the National Covid-19 Traveller Service User Experience Survey, published by the NSIO in October 2020, a combined 85.6 per cent of Travellers accessed information on Covid-19 through local Traveller projects and Traveller health units.
Pavee Point’s long-running Traveller primary healthcare project (TPHCP) also aided Safetynet and the HSE in providing help to the Traveller community, according to TPHCP Assistant Coordinator Ms Mary Brigid Collins. “I don’t think that the HSE would be able to do what they actually did out the ground without the support of the primary healthcare project,” Ms Collins told MI.
“Because the primary healthcare projects have been going on since 1994 and we have the trust and relationship built out there with lots of Travellers.”
The TPHCP comprises Travellers who identify the health needs of the community. It aims to develop the skills of Travellers in providing community-based health services; liaising and assisting in dialogue between Travellers and health service providers; and highlighting gaps in health service delivery while working towards reducing inequalities that exist in established services.
Lack of data
There is concern, however, that the lack of accurate, disaggregated data based on ethnicity will continue to hinder progress in addressing Traveller health inequalities.
The HSE collected ethnic data on those who tested positive for Covid-19 from the second wave of the virus in August 2020 onward.
“At local level, also, some public health medical specialists were able to verify those as Travellers through their direct links and with Traveller health unit primary care workers,” a HSE spokesperson said. “Capturing ethnicity was not always done during Covid peaks especially if there were high caseloads of positive Traveller patients.”
Within the Covid case ethnic identification, “we also noted that there was a massive undercount,” Ms Kavanagh of Pavee Point told MI.
“We would say that Travellers and Roma were disproportionately impacted by Covid-19 alongside other marginalised groups,” she said. “And that those particular consequences aren’t captured in official datasets, because we don’t have disaggregated data on the basis of ethnicity or ethnic equality monitoring.”
HIQA reported in March 2021 that Travellers were more at risk of contracting the virus than the general population. However, HIQA also said “limitations in the data relating to these hard-to-reach groups means that the estimates presented are considered to underestimate the true prevalence”.
Ethnic identifiers were also not embedded into the vaccination information system.
The concern around data extends beyond the pandemic.
“What we do need is an ethnic equality monitoring right across the health services and other Government and statutory agencies,” Ms Kavanagh added. “So that we’re able to join up the dots and then we’re not sitting another 15-20 years from now saying, ‘Look, do we need another piece of research?’”
The most robust data collection regarding Traveller health was in 2010 in the AITHS.
Dr Fitzgerald told MI: “The findings in the AITHS are still valid and any further research in recent years has confirmed that the findings are valid and the gap is widening in terms of the health status and life expectancy of Travellers.”
The November 2021 joint Oireachtas committee on key issues affecting the Traveller community reported: “The vast majority of the witnesses who appeared before the joint committee and those who made submissions called for the adoption of an ethnic identifier to allow for accurate information, better social policy and service planning.”
Implementing ethnic identifiers was also recommended in the NTRIS and the AITHS.












Leave a Reply
You must be logged in to post a comment.