While new figures show increasing consultant numbers, representative bodies say recruitment
and retention difficulties endure. David Lynch reports
Consultant recruitment is on the rise, according to new figures from HSE National Doctors Training and Planning (NDTP).

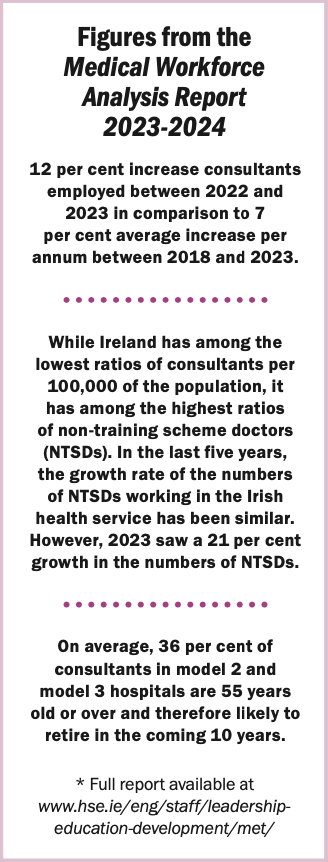
Some standout statistics in the NDTP’s Medical Workforce Analysis Report 2023-2024 include: A 12 per cent rise in the overall number of consultants employed last year; a 16 per cent growth in the number of consultants employed in model 3 hospitals; and a 4 per cent rise in the number of doctors in training.
NDTP Medical Director Prof Brian Kinirons told an online webinar last month the report was important “because there is a national narrative that many of our doctors are leaving the country and not coming back to work to Ireland and of course… it is much more nuanced than that”.
The webinar saw the NDTP launch both its new analysis report and the Annual Medical Retention Report 2023.
During her presentation on the analysis report, Ms Aimée Maguire from HSE Medical Workforce Planning said there was an average annual 7 per cent growth in consultant numbers between 2018 and 2023. However, in 2023 the rate rose to 12 per cent. “So that’s a good sign and a good move in the right direction to achieve a consultant-delivered service,” she said.
Ms Maguire noted that emergency medicine, in particular, enjoyed “quite a substantial growth in the number of consultants”.
“This is likely due to the increase in number of consultant posts approved in 2022 for emergency medicine… as part of the HSE Winter Plan for emergency department staffing.”
Model 3 hospitals
Ms Maguire highlighted that both the model 3 and model 4 hospitals had seen “substantial growth” in consultant numbers during 2023.
“The model 3 growth rate was 16 per cent in [the] last year; this would suggest that there was a large recruitment drive of consultants to these model 3 hospitals.”
In 2023, the NDTP launched a report on medical staffing in model 3 hospitals. It outlined the serious recruitment difficulties faced by these hospitals and explored ways to improve consultant recruitment at these sites.
“So this growth is really a good step in the right direction,” said Ms Maguire.
Considering the challenges within the sector, the increase in model 3 hospital consultant recruitment last year may come as a surprise.
“I don’t think it was predicted,” said Mr Tom Pierse from the NDTP in response to a question from the Medical Independent (MI) during the webinar.
He cited the introduction of the public-only consultant contract (POCC23) as “one of the potential causes”. But he said there was likely to be “societal reasons” as well. For instance, property prices are often cheaper in areas with model 3 hospitals, which are typically located away from major urban areas.
However, he pointed out “we don’t actually have data around what the causes are”.
Regarding NCHDs and training, the analysis report said there was a 4 per cent growth in the number of doctors in specialist training and a 21 per cent increase in the number of doctors in non-training posts between December 2022 and December 2023.
This increase in doctors in non-training posts has been highlighted by the NDTP as a particularly problematic issue (see panel p5).
Vocation
However, despite some of these positive looking trends, representative bodies and researchers in the area continue to underline that significant impediments remain regarding consultant recruitment
and retention.
The hospital doctor retention and motivation (HDRM) project has gathered and published considerable data in recent years.
The project’s most recent research was published early this year in SSM – Qualitative Research in Health. The research focused on the working conditions of Ireland’s hospital doctors and asked whether their core work needs are being met and whether ‘medicine as vocation’ is used to excuse poor working conditions.
Co-author of the paper, Dr Niamh Humphries (PhD), Senior Lecturer at the RCSI Graduate School of Healthcare Management, told MI that it is important hospital doctors are afforded the same employment rights as other employees.
She said this means being able to achieve a work/life balance and maintain their wellbeing while working in the Irish health system.
“I think these things are essential if we want to improve doctor retention in the Irish health system,” added Dr Humphries. “I think sometimes there’s a perception that the privilege of practising medicine is reward enough and that somehow employment rights don’t apply to hospital doctors.”
The narrative of “medicine as vocation” seems a strong one in society. So where should the impetus come to promote the concept that doctors are also employees and workers?
Dr Humphries said how this will be addressed is an “interesting question”.
“I think first and foremost it’s an issue for the HSE and healthcare management,” she said. It is the responsibility of management, she argued, to ensure that “staffing levels and rotas for hospital doctors are designed around manageable workloads and reasonable working hours”.
“I also think that improved working conditions is an issue that the postgraduate training bodies, unions, and medical schools need to advocate for on behalf of current hospital doctors and the future medical workforce.”
Adrift
The HDRM’s paper also noted that hospital doctors in Irish hospitals “experience minimal line management”.
Reflecting on this finding, Dr Humphries noted that a line manager plays an important role in any organisation. “Especially in relation to allocating work, ensuring
that workloads are manageable and providing leadership.”
“They connect the employee to the organisation, ensuring that the organisation is aware of the issues facing the employee and that the employee is aware of organisational priorities.”
Dr Humphries told MI that “if that role is missing in hospitals, it leaves hospital doctors adrift from an organisational perspective”. In such cases, doctors feel that no-one in the organisation “understands their perspective, or advocates for them and they have no one to turn to” if they face challenges.
Unsafe
In a statement to the joint Oireachtas health committee last month, the IMO said the current HSE recruitment embargo had led to an increase in “illegal and unsafe working hours”. The Organisation pointed out that 83 per cent of NCHDs are now routinely working beyond 48 hours per week.

In relation to consultants, IMO representatives also told the committee that consultants “are often appointed to a position with no admin support, no office, no team members, insufficient or no clinic times, no theatre time, and challenges in accessing diagnostics”.
The IHCA informed MI that it welcomes any increase in consultant numbers, such as those indicted in the recent NDTP reports. However, a spokesperson for the Association said: “We have called on the Government to fund and appoint 2,000 additional permanent consultants by 2030 – or around an extra 350 annually.”
The spokesperson said the NDTP figures show that the number of consultants “employed on a non-permanent basis actually rose to a record 643 in 2023 – an increase of 24 per cent compared with the previous year”.
Demands
The HSE “has previously acknowledged” that an increase of 1,876 in the number of consultants working in acute hospitals is required by 2028, according to the Association.
“However, the continued resourcing and capacity deficits in the health service does not help this recruitment. The working conditions for hospital specialists and the functionality of the health service must be improved if we are to retain NCHDs and consultants and encourage those emigrant doctors to return to Ireland.”
The “fallout” from the Covid-19 pandemic and the ongoing hospital crowding crisis have placed even more “extreme work demands” on consultants and other frontline staff, according to the spokesperson.
A 2023 survey of IHCA members found 69 per cent of consultants experienced symptoms of burnout due to work pressures in the previous 12 months.
Additional medical team supports “are also urgently needed” for consultants to provide an effective and efficient service. “Those consultants who leave Irish public hospitals to work abroad or in the private sector often cite the stress of trying to maintain an effective and efficient service with an inadequately staffed medical team as a major factor in their decision to leave. All of these issues need to be addressed to tackle the continuing recruitment and retention difficulties facing the public health service.”
*The HDRM paper is available at www.sciencedirect.com/science/article/ pii/S2667321524000015
Consultants in psychiatry: Coping with a ‘surge’
In May, the IHCA highlighted that around 3,760 children and adolescents are awaiting an appointment with the HSE’s child and adolescent mental health service (CAMHS). The Association said this was a 62 per cent increase compared with pre-pandemic levels.
The IHCA pointed to HSE figures showing 28 per cent of consultant psychiatry posts were vacant or filled on a temporary basis. More than one-in-three CAMHS psychiatry posts were not filled as needed.
The Medical Independent (MI) asked the IHCA whether there are any specific measures that could help recruitment of consultant psychiatrists.
“Deficits in staffing and resources, especially the scarcity of adult acute mental health beds in Ireland is making it harder to retain mental health specialists,” IHCA Vice-President and Consultant Liaison Psychiatrist, Prof Anne Doherty, told MI.
She added that with only 23.8 adult acute mental health beds per 100,000 population in public approved centres in Ireland, compared to the EU mean of 73 per 100,000 population, “many doctors are left agonising over whether to stay in this country, or to move abroad for better working conditions.”
“When I graduated from medical school in 2005, there were 4,000 acute mental health beds in Ireland,” she said. “That number has now decreased to around 1,100.
“In real terms, what that means is that for every four patients we would have admitted to hospital in 2005, we would only admit one today. As such, inpatient psychiatric care is now reserved only for the ‘seriously ill’.”
She said that Ireland trains enough doctors in the specialty every year.
“But the problem is, like with every other area of medicine in Ireland, psychiatrists are leaving for or remaining in other English-speaking countries, where they have enhanced working conditions and the health service functions better.
“It’s very difficult for Irish doctors to decide to come home and, for example, make those very difficult choices of who gets that single mental health bed when you have four people who need it.”
Prof Doherty added that the country “urgently” needs to recruit highly trained specialists to fill the “large proportion” of vacant consultant psychiatry positions nationwide.
She identified another factor which is “demoralising and forcing our specialists to work abroad, or even leave the profession altogether”. This is the stress of having to “constantly battle against the realities of a health service that, due to staffing and resource deficits, can prevent the delivery of care at a high standard and in a timely way”.
Prof Doherty said this “moral distress” can take a heavy toll on doctors’ wellbeing and contribute to “exits from Ireland or the profession”.
Continuing ‘over-reliance’ on non-training doctors
The HSE National Doctors Training and Planning (NDTP) Annual Medical Workforce Analysis Report 2023-2024 reported a 21 per cent increase in the number of non-training NCHDs working in the health service in 2023.
As part of a recent NDTP online webinar, the Medical Independent asked the programme’s Medical Director Prof Brian Kinirons what impact this sharp increase has on the health service.
Prof Kinirons replied that “we are moving in the opposite direction” of HSE policy on this issue.
“That policy is really around reducing our reliance on non-training scheme doctors and Ireland has a unique reliance on non-training scheme doctors in a way that no comparative country has.”
He said this growth is driven by different factors. These include the need to comply with the European Working Time Directive and to meet the demand within unscheduled care.
“So specialties such as obstetrics and paediatrics, intensive care medicine, emergency medicine are all driving… the need for these non-training scheme doctors.”
Prof Kinirons added that another challenge is that the recruitment of non-training doctors takes place “at a local level, so it is a response to local service requirements”.
However, he hopes that this over-reliance will be reduced by increasing the number of consultants.
Asked whether this increase in non-training scheme doctors will continue in the coming years, Prof Kinirons said that “certainly history would suggest we have been unable to control this to date and it is a difficult piece to control”.













Leave a Reply
You must be logged in to post a comment.