Bette Browne examines the reasons why US medical professionals are leaving the profession in alarming numbers
The Irish health service is not the only one facing a recruitment and retention crisis.
Staffing challenges exist in healthcare services across many countries. In the US, for instance, medical professionals are leaving the profession in their thousands.
The exodus means an estimated shortage of between 37,800 and 124,000 doctors by 2034, including shortfalls in both primary and specialty care, according to a recent study by the Association of American Medical Colleges (AAMC).
Total projected shortages by 2034 will vary by specialty grouping, found the 2021 study. There will be a projected shortfall of between 17,800 and 48,000 primary care physicians and a shortfall of between 21,000 and 77,100 non-primary care physicians, including between 15,800 and 30,200 surgical specialists.
The AAMC’s study, ‘The complexities of physician supply and demand: Projections from 2019-2034,’ was a wake-up call on the crisis in the midst of the Covid-19 pandemic.
“The Covid-19 pandemic has contributed to a rising physical and emotional toll on physicians and other health professionals. The ongoing crisis has also exposed vulnerabilities in the healthcare system that led to some healthcare workers being furloughed or facing financial hardship,” the study noted.
“The evidence shows that health workers have been leaving the workforce at an alarming rate over the past two years,” Mr Thomas R Cunningham, a senior behavioural scientist at the National Institute for Occupational Safety and Health, told the Journal of the American Medical Association on 30 March 2022.
Overall, more than a quarter of a million doctors, nurse practitioners, and other clinicians left the US healthcare workforce in 2021 alone, according to a report last October by Definitive Healthcare, which compiles information and statistics on US medical institutions. It also found that one-in-five doctors, who are currently practising, plan to leave the profession sooner rather than later.
The report looked at which specialties have been most impacted by staffing shortages. It found that internal medicine and family practice were among those which experienced the greatest turnover throughout 2021.
The shortage of healthcare workers is certainly not unique to the United States. Indeed, the World Health Organisation estimates a projected worldwide shortfall of 10 million healthcare workers by 2030, mostly in low- and lower-middle income countries. Yet it is a shortfall that should not be approaching what the AAMC calls “critical levels” in a wealthy country like America.
Causes
So why is it such a problem in the US? The causes are diverse, as they are in other countries. However, in the US, they are further exacerbated by socio-economic inequalities that are deepening rather than lessening amid growing political polarisation.
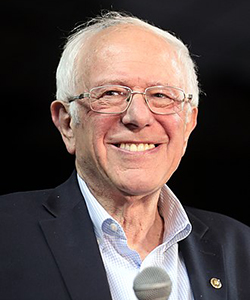
In 2017, the former US Presidential hopeful, Senator Bernie Sanders, termed the country’s healthcare system as dysfunctional. “It’s about whether we maintain a dysfunctional system that allows the big drug and healthcare companies to make over $100 billion in profit last year. All the while one out of five Americans cannot afford to get the prescription drugs that their doctors prescribed.”
Some might disagree with how Senator Sanders framed the problem, but US polls show most believe their healthcare system is seriously broken and needs to be fixed. A poll last September by the Associated Press and the Chicago-based National Opinion Research Centre found less than half of Americans expressed satisfaction in the system.
Inevitably, staff shortages, demoralisation and burnout also put patients at risk. With fewer healthcare professionals on staff, the likelihood of a medical error can increase. A study from Johns Hopkins Medicine in 2016 suggested that medical errors were the third leading cause of death in the US, accounting for more than 250,000 deaths annually. More recently, the Harvard Business Review reported in April 2022 that an estimated 1.2 million are harmed each year by medical errors.
Many of these issues are contributing to demoralisation among doctors, who are already suffering burnout. The President of the American Medical Association (AMA), Dr Jack Resneck, along with US Surgeon General Mr Vivek Murthy, addressed the issue of physician burnout at a webinar organised by the AMA on 9 March this year.

“Many factors drive burnout in the practice of medicine, a complex and pervasive issue with widespread implications for both physicians and patients,” Dr Resneck said. “The AMA is leading the national effort to solve the growing physician burnout crisis. We’re working to eliminate the dysfunction in healthcare by removing the obstacles and burdens that interfere with patient care. In short, we need to fix what’s broken in healthcare today – and it’s not the doctor.”
But other doctors say the causes of demoralisation are even more fundamental. This was emphasised in a hard-hitting analysis by Dr Eric Reinhart, a political anthropologist and physician at Northwestern University, outside Chicago, who explained the emergence of what he called ‘demoralisation syndrome’ among US doctors.
“Doctors have long diagnosed many of our sickest patients with ‘demoralisation syndrome’ a condition commonly associated with terminal illness that’s characterised by a sense of helplessness and loss of purpose,” Dr Reinhart wrote in the New York Times in February. “American physicians are now increasingly suffering from a similar condition, except our demoralisation is not a reaction to a medical condition, but rather to the diseased systems for which we work.
“The United States is the only large high-income nation that doesn’t provide universal healthcare to its citizens. Instead, it maintains a lucrative system of for-profit medicine. For decades, at least tens of thousands of preventable deaths have occurred each year because healthcare here is so expensive.
“During the Covid-19 pandemic, the consequences of this policy choice have intensified. One study estimates at least 338,000 Covid deaths in the United States could have been prevented by universal healthcare. In the wake of this generational catastrophe, many healthcare workers have been left shaken.”
Citing the fact that 117,000 doctors left the US healthcare workforce in 2021 while just 40,000 joined it, Dr Reinhart said the exodus could not be explained by burnout alone. It was far more fundamental, he suggested.
“The burnout rhetoric misses the larger issue in this case: What’s burning out healthcare workers is less the gruelling conditions we practise under, and more our dwindling faith in the systems for which we work. What has been identified as occupational burnout is a symptom of a deeper collapse. We are witnessing the slow death of American medical ideology.”
He concluded that nothing short of a fundamental overhaul of the country’s healthcare systems would suffice.
“Doctors can no longer be passive witnesses to these harms. We have a responsibility to use our collective power to insist on changes: Universal healthcare and paid sick leave, but also investments in community health worker programmes and essential housing and social welfare systems. To be able to build the systems we need, we must face an unpleasant truth: Our healthcare institutions as they exist today are part of the problem rather than the solution.”
The political climate is also part of the problem. Many doctors and healthcare workers, along with their patients, were dismayed last year when the US Supreme Court overturned the federal right to abortion. They felt it gravely endangered women’s health and some doctors were fearful they could be at risk of legal action in a number of states if they continued to advocate for their patients’ health and safety.
This was also on the mind of Dr Resneck at the AMA webinar. “My physician colleagues now face anti-science aggression by some in positions of power and influence, along with a well-coordinated onslaught of medical disinformation from social media and other channels. At the same time, we’re fighting efforts by some to interfere with decisions made between doctors and patients in our exam rooms. The recent criminalisation of comprehensive reproductive healthcare in many states following the (Supreme Court) decision has been accompanied by increasing hostility and threats directed at physicians and other medical workers.
“Taken together, these factors create a toxic environment that hampers physicians’ ability to do what drew us to medicine in the first place, deliver high-quality, compassionate care to our patients. Most of us haven’t lost the will to do our jobs, but we’re frustrated that our healthcare system just puts too many obstacles in our way. The result is physician burnout. It’s real and it’s rising,” Dr Resneck told the webinar.
Surgeon General Mr Murthy agreed, citing the growing number of clinicians affected by mental health concerns. “This is not the concern of 1 per cent or 2 per cent. The vast majority of clinicians at some point experience mental health struggles, whether it’s depression or anxiety, challenges with managing stress or with handling the loneliness and isolation that sometimes can come with our work.

Mr Vivek Murthy
“Our colleagues are struggling and they’re suffering. And it’s not only them that are on the line, but it’s the patients they care for, who they care for, whose health is now at risk and whose access is at risk. So health worker burnout is not just a problem for health workers. This is a national priority and it’s one that deserves our collective attention.”
Racial disparities
Lack of diversity among the medical workforce is also a major issue in the US, according to the AAMC. “There has been minimal progress in increasing the number of physicians from diverse racial and ethnic backgrounds,” the Association’s President Dr David Skorton told a US Senate committee in 2021 at a hearing titled ‘A dire shortage and getting worse: Solving the crisis in the healthcare workforce’.
“We need more assertive efforts to cultivate a more diverse and culturally prepared workforce. We must design bolder interventions to address the growing absence of black men and the near-invisibility of American Indians and Alaska Natives in medical school and the physician workforce, which are national crises.”
Racial disparities in the system are also a major concern. Black and Hispanic adults in particular are extremely worried about healthcare access, with nearly six in 10 saying they are very or extremely concerned about getting good care. Fewer than half of white adults, 44 per cent, expressed the same level of concern in the AP-NORC poll.
Such disparities have long plagued America’s healthcare system. They became abundantly clear during the Covid-19 pandemic, with black and Hispanic people dying disproportionately from the virus. A report in August 2022 by the Centres for Disease Control and Prevention (CDC) found minorities faced about one-and-a-half times greater risk of Covid infection than white people, and were about twice as likely to die from the disease as their white counterparts.
Covid-19
A state-by-state analysis on Covid’s impact, published in The Lancet in March, revealed how the pandemic played out in vastly different ways in states across the country. “Although the USA has the largest economy, spends more on healthcare than any other country, and was ranked as best prepared for a pandemic in the Global Health Security Index in 2020, it maintains the highest number of recorded Covid-19 deaths and one of the highest per capita fatality rates from Covid-19 globally. But the pandemic did not impact US states equally,” the analysis noted.
“The tragic human toll of the Covid-19 pandemic in the USA challenged conventional assessments of pandemic preparedness and exposed existing vulnerabilities in our societal fabric that were not identical across states,” said co-lead author Ms Emma Castro, a researcher at the Institute of Health Metrics and Evaluation. “Even after accounting for age and underlying illnesses, we observed a nearly four-fold difference in Covid-19 death rates across states.”
Racial disparities and the political climate were largely to blame for this, according to co-lead author Mr Thomas J Bollyky, Director of the Council on Foreign Relations’ Global Health Programme in the US. “A combination of racial disparities and politics explains a large part of why the USA particularly struggled in the pandemic. To rebuild trust in public health and the future pandemic response, we must improve transparency around the political contexts and social, economic, and racial inequities that have magnified US struggles in this crisis.”
Affordable care?
Moves by Congress to address these issues have failed to make any real progress. President Barack Obama’s Affordable Care Act in 2010 succeeded in making insurance affordable to millions of those who had no insurance. But instead of expanding its provisions, as had been planned by Democrats in the decade that followed, Republicans in Congress continually sought to overturn the Act or block it in court challenges, albeit unsuccessfully.
In addition, this year patients and their doctors are increasingly concerned that changes could be proposed in Congress that would see cuts to key federal medical aid programmes – Medicare for older persons and Medicaid for people on low incomes – along with social security entitlements.
Covid supports that ensured millions were covered by the Medicaid programme are now being withdrawn. This “re-determination” process started in April, when states began to check the eligibility of the 90 million people currently on Medicaid to confirm they still meet the criteria for benefits. If, for example, state officials cannot reach someone because the person moved or didn’t check a notice from the state, that person could be eliminated from Medicaid.
Preventing this worst-case scenario will depend on states making every possible effort to reach people, so Congress has given states up to 12 months to complete the re-determination process. But in Texas, where as many as one million people may lose coverage, state officials have said they want to finish the process in eight months.
The popular Medicare programme for older persons could also be threatened. President Joe Biden’s $6.8 trillion proposed budget, released by the White House in March, singled out protecting Medicare as one of his top priorities in the face of suggestions by some Republicans of making changes over time to the programme.
The dispute is in the context of an ongoing debt ceiling debate. Republicans have publicly said they want to make spending cuts, but there’s a major divide on what they want to cut. Medicare and social security are off the table, according to the Speaker of the House of Representatives Kevin McCarthy. But the White House is not convinced and President Biden has vowed to protect these landmark programmes.
So instead of also being expanded to all Americans, as proposed by Senator Sanders and 14 of his colleagues in the Senate one year ago when they introduced the Medicare-for-All Act (MAA), action has been stalled because the votes are not there to pass it. The Bill was hugely popular in polls and doctors said it could have transformed healthcare access in the US.
“The MAA has the potential to transform the availability and efficiency of American healthcare,” a group of doctors said in a paper titled ‘Improving the prognosis of healthcare in the United States’, which was published in The Lancet in February 2020, when it seemed the Act might get sufficient support in Congress.
The doctors also said it would make sound financial sense. They calculated that a single-payer, universal healthcare system as proposed in MAA would lead to a 13 per cent saving in national healthcare expenditure, equivalent to over $450 billion annually.
“This shift to single-payer healthcare would provide the greatest relief to lower-income households. Furthermore, we estimate that ensuring healthcare access for all Americans would save over 68,000 lives and 1.73 million life-years every year.” However, they cautioned that “strong opposition should be expected from powerful vested interests, including the health insurance and pharmaceutical industries”.
“Counterbalancing these concerns is the moral imperative to provide healthcare as a human right, not dependent on employment or affluence. We should seize this opportunity to promote wellbeing, enhance prosperity, and establish a more equitable healthcare system for all Americans.”
So far, however, such vested interests have prevailed and another opportunity for fundamental change has been stymied.













Leave a Reply
You must be logged in to post a comment.