As negotiations for a new public-only contract look set to recommence, Paul Mulholland explores the latest data concerning private activity and the HSE’s attempts to monitor the area.
The issue of the private practice activity of consultants working in public hospitals has been a source of tension for some time.
In 2017, the HSE hired private investigators in relation to alleged non-compliance of public/private ratios by consultants under the terms of the 2008 consultant contract. The action was instigated in the context of defending 10 ‘lead’ High Court cases taken by consultants for pay increases due under the contract.
The Department of Health and the HSE lost the litigation proceedings. The estimated cost of the June 2018 settlement was €182 million for arrears and ongoing costs of €62 million per annum from 2019.
Shortly before the settlement was reached, in April 2018, the Department asked the HSE to establish a framework to ensure compliance with the terms of the consultant contract regarding private practice. The Department requested the HSE’s internal audit division be consulted on the establishment of the framework and that consultant compliance form part of the Executive’s annual internal controls process. It was also requested that the HSE’s audit committee be asked to include consultant contract compliance in its work programme.
Before 2014, compliance with the contract had national oversight. However, in 2014 this was delegated to the Hospital Group CEOs. The new framework was intended to re-introduce oversight at a national level.
In addition, the 10-year health strategy, Sláintecare, published in 2017, recommended the removal of private practice from public hospitals. This has formed the basis for a proposed new public-only contract. Engagement with consultant representative bodies on this contract has been protracted and difficult (see panel).
Compliance with public/private mix
A number of annual reports have now been produced under the new framework, all of which have been obtained by the Medical Independent (MI) through Freedom of Information (FoI) law. They show that overall consultants have, in general, worked below the 20 per cent threshold for private activity specified in the contract.
This trend has continued in the 2020 annual report, which is the most recent report to have been completed.
However, the Covid-19 pandemic proved an obstacle in terms of data collection.
“[The] progress that had been achieved towards the timely reporting of compliance with private activity limits stalled in 2020 due to the effects of the pandemic on activity and staffing in hospitals,” according to the annual report.
Following requests from a number of hospitals the requirement to submit the data was suspended between March and October 2020. As a result, the 2020 data was not finalised until the third quarter of 2021. A number of Hospital Groups had also been further impacted by the cyberattack last year.
According to the data collected, the level of private activity reduced across the Hospital Groups in 2020. This was due to the impact of Covid on both elective admissions and emergency attendances in the year. Patients did not have the option to avail of private care for Covid treatment.
The need to ensure public hospitals were sufficiently staffed with medical personnel during the pandemic also had an impact on private activity during this time.
“Given the impact of Covid on the level of private practice/activity, the Department approved the HSE temporarily offering consultants the facility to switch from their ‘permanent’ contracts – that permitted private practice – to Type A ‘public-only’ contracts,” according to FoI correspondence.
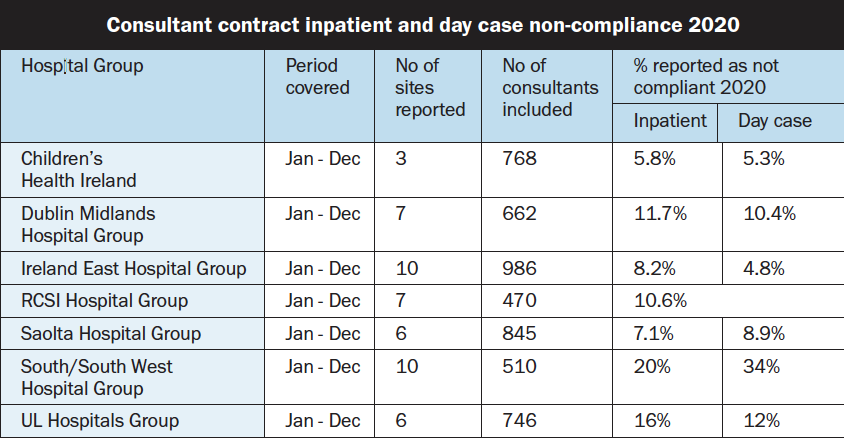
The new data, obtained by MI, show that the highest percentages of non-compliance was in the South/South West Hospital Group (SSWHG). Out of the 510 consultants included, 20 per cent were reported as non-compliant in relation to inpatients, and 34 per cent were non-compliant in relation to day cases. SSWHG was followed by University of Limerick Hospitals, in which, out of the 746 consultants included, 16 per cent were non-compliant in relation to inpatients, and 12 per cent in relation to day cases (see table for the full Hospital Group breakdown).
No cases of consultant non-compliance were escalated to the National Director of Acute Operations in 2020.
“While the assessment of overall public private mix is a separate issue, the percentage of private discharges in 2020 of 13.1 per cent (2019 – 13.9 per cent) is below the 20 per cent threshold [and] is evidence of general adherence to the limits,” according to the annual report.
Emergency admissions
As with previous reports, a number of factors were highlighted as being largely outside of the control of the hospitals/consultants in contributing to levels of public/private activity.
Chief among these is the issue of emergency admissions. The level of private work in public hospitals was addressed in 2018 in a report by the Comptroller and Auditor General (C&AG). The C&AG concluded that, in practice, the HSE, hospitals and individual consultants have limited control over the private activity levels as the majority of patients admitted to hospitals come through the emergency departments or are maternity admissions. These patients must be admitted and treated in order of clinical priority.
“In these cases, the consultant on call is assigned the patient irrespective of the patient insurance status and therefore it is outside of the consultant’s control,” the 2020 annual report stated in relation to emergency admissions.
“To put this into context, 70 per cent of all inpatient discharges in 2020 were admitted on [an] emergency basis.” In 2019, the corresponding proportion was 69 per cent.
In 2020, some 564,905 inpatient discharges took place, compared to 635,532 in 2019. While 70 per cent were admitted on an emergency basis, when maternity discharges are excluded the percentage of emergency discharges increases to 86 per cent. Notwithstanding the high proportion of emergency admissions, the level of private inpatient discharges was 16 per cent in 2020. In 2019, the percentage was 15.7.
Other factors
Other factors that contribute to private activity include the specialist services that the hospital provides, and whether it is a larger hospital providing emergency and complex care or a smaller hospital with less complex emergency, day case, and elective care.
In relation to tertiary and specialist services, “patients are typically managed in a small number of centres.”
“This can result in a higher proportion of private patients/complexity for the relevant consultants than their limit allows,” according to the document.
Another factor to consider is whether comparable services are available in a nearby private hospital. Where there is no private hospital located in the same region as the public hospital, all required private work will be carried out in the public hospital.
There is also the issue of whether the consultant holds a post on a split appointment basis.
“If consultants in the hospital hold split appointments in that they work over two or more hospital locations – a high ratio of private activity in one location may be offset by a low ratio in another location,” according to the report.
The completeness of hospital inpatient enquiry (HIPE) system coding can have an impact on the overall compliance reported. The annual report also notes another issue in relation to HIPE.
“Workload which is coded in HIPE as a consult (other consultant review and advice usually on a once-off basis and patient remains under the care of the admitting consultant) may result in consultant compliance changes as part of the HIPE coding process,” according to the annual report.
“This can be misleading and, in some cases, Type A [public-only] consultants, having what would appear as a contract breach.”
Data can also appear skewed if the consultant in question only has a small number of discharges during a reporting period.
The annual report states mechanisms are required to include outpatient and diagnostic activity so that overall compliance can be measured more effectively.
“No effective mechanism has been identified to date,” according to the document.
Framework audit
The consultant contract compliance guidance framework had been largely finalised by early 2020 and data collation and reporting by hospitals and Hospital Groups was broadly in line with the rules.
In January 2020, the HSE internal audit division had reported to the National Director of Acute Operations on the effectiveness of the compliance framework. The report included 10 findings and 13 related recommendations. At the end of 2020 there were five recommendations yet to be implemented.
The first was to “review, and as appropriate, update the national policies and procedures for the management of and compliance with consultant contracts”. Work was also to be undertaken to agree and implement an approach to measure outpatient and diagnostic activity.
“No progress was made to date because of the pandemic,” stated the annual report.
A standard work practice plan and related processes were also to be implemented. Other issues/recommendations to be discussed were the implementation of a “consultant compliance annual declaration process” with regard to onsite and offsite private practice and the development of a “detailed training module”, covering all aspects of the reporting framework.
The framework was referred by HSE acute operations to the national human resources division in the third quarter of 2020 in order to facilitate engagement with consultant representative bodies.
MI understands there has been limited engagement regarding these matters since 2020.
A spokesperson for the HSE confirmed there has been no movement on the audit recommendations over the last year.
Most of the recommendations are dependent on the first recommendation on finalising the framework and engagement with the medical unions.
“Due to the impact of the pandemic on hospital services and discussions in relation to the Sláintecare contract, wider discussions are to take place,” the HSE spokesperson told MI.
2021
The HSE is currently working on the annual report for 2021.
According to the FoI response, the Department continued to be in contact with the relevant sections of the HSE in relation to private practice over the past year.
“Again, private activity in 2021 (and public) was impacted substantially by the need to organise the acute system and care pathways to deal with Covid and the HSE continued to offer consultants the facility to avail of Type A contracts on a temporary basis,” stated the FoI correspondence.
Over 150 consultants availed of this facility, according to the correspondence.
A Department of Health spokesperson told MI that the compliance framework remains a priority, despite the plans for a new contract.
“The Sláintecare contract will be the only contract available to future consultants from the implementation date and will result in a phased removal of private practice from the public system over time,” according to the spokesperson.
“Consultants who hold contracts that allow them engage in private practice, the majority of serving consultants, will continue to be subject to the framework.”
The long journey towards a new contract
The removal of private practice from public hospitals is a key part of the health reform programme under Sláintecare. The strategy, which was published in May 2017, called for the “phased elimination” of private care in public hospitals. However, it also called for an independent impact analysis of the separation of private practice from the public system in order “to identify any adverse and unintended consequences on the public system”.
This analysis (the Report of the Independent Review Group established to examine private activity in public hospitals) was eventually published in August 2019, after some delay. The report recommended the creation of a public-only (Sláintecare) contract and for the introduction of legislation to ensure that public hospitals are exclusively used for the treatment of public patients from the conclusion of the 10-year Sláintecare implementation period.
In December 2019, the then Minister for Health Simon Harris and Minister for Finance, Public Expenditure and Reform Paschal Donohoe announced “a new Sláintecare contract for consultants”.
From quarter two of 2020, all future consultant appointments were to be offered the new contract, which would require consultants employed by the State to focus 100 per cent of their time on public-only work.
Reflecting this change, the Sláintecare contract was to be offered at increased pay levels of up to €222,460, rising further to €252,150 by July 2022.
Existing consultants were to be offered the opportunity to switch to the new proposed contract but would retain the option to remain on their existing contract.
The day before the announcement, IMO consultant and NCHD members had voted in favour of industrial action (ultimately this never went ahead).
“Clearly yesterday’s overwhelming vote by IMO consultant and NCHD members to vote in favour of strike action in the New Year is already having an impact in terms of engaging the Taoiseach in this crisis,” the IMO stated at the time.
“However, the Taoiseach must understand that to resolve this issue will require negotiations with the IMO and not unilateral pronouncements in the Dáil.”
While the IHCA welcomed the Government’s acknowledgement of the consultant recruitment crisis, it also reacted sceptically to the announcement. The Association stated the plans to remove private practice from public hospitals “will create an annual funding hole of €650 million in cash-starved public hospitals and wreak havoc on patients”.
The Government’s plan to introduce the new contract in 2020 did not materialise and there was no progress over the next year and a half as the country battled the Covid-19 pandemic.
The “unilateral” approach of health management continued to be a source of contention for consultant representative bodies.
In May 2021, in a bulletin to members, the IMO stated the Department of Health’s position was that matters relating to the contract were not for negotiation. According to the Organisation, the Department had sought to bypass negotiations and engage only in an “information and feedback” process.
When details of the draft contract were released in June, the reaction from consultants and NCHDs online was overwhelmingly negative.
Substantive negotiations began in September, with the appointment of an independent Chair Ms Marguerite Bolger viewed as key to the process by both the IHCA and the IMO.
At the IHCA’s AGM in October 2021 Minister for Health Stephen Donnelly said he was “keen to see a new contract agreed within weeks”.
However, progress was slow. Talks broke down in December and the failure to replace Ms Bolger, who was appointed as a High Court judge in January, has held up the process this year.
Minister Donnelly continued to strike an optimistic tone, saying recently that he hoped for the new contract to be introduced this year.
He also referred to recent “progress” on the issue of re-engagement during his speech at the IMO AGM on 28 May. The Organisation’s CEO Ms Susan Clyne had earlier told the national consultant meeting that it was expected a new independent Chair for negotiations would be appointed soon.
“We do need it agreed this year, it has to be agreed this year,” the Minister said in response to a question from MI on when a contract would be finalised, given the delays that have occurred to date.
“…. I believe that there is a very attractive, new public contract that is true to the Sláintecare principle of taking private work out of our public hospitals.”
The recently published Sláintecare Action Plan 2022 also states the intention for progress on the issue to be made this year, even if it falls short of saying exactly when a new contract would be introduced.
Project 7 under the action plan refers to the removal of private care from public hospitals and the introduction of a Sláintecare contract. There are two ‘deliverables’ under this workstream. The first is to “provide Government update on Sláintecare consultant contract on negotiations with representative bodies” (quarter two). The second is to “progress plans to remove private care from public hospitals, subject to agreement with representative bodies on the introduction of the Sláintecare contract” (quarter four).













Leave a Reply
You must be logged in to post a comment.