Quality-of-life in osteoporosis is
currently not measured adequately and this needs to change to improve outcomes
in these patients, the ISR Autumn Meeting heard.
UK expert
on quality-of-life in patients with arthritis and osteoporosis Dr Marwan
Bukhari, Consultant Rheumatologist and Clinical Lead for Rheumatology at the
University Hospitals of Morecambe Bay NHS Foundation Trust, pointed out how
quality-of-life measures in more symptomatic diseases like rheumatoid arthritis
(RA) are seen as important but not so much in osteoporosis, where fracture
incidence/prevention is the primary measurement.
“People
without a fracture [who have osteoporosis] are really quite rare and in fact
the definition of osteoporosis is quite interesting, because it was in
post-menopausal women above the age of 50. Now, how many of you will have seen
a DEXA scan of someone aged 40 of -2.5 and called them osteoporotic? Probably
everybody, and how many of you have seen a bloke with a T-score of -2.5
anywhere and called them osteoporotic? Probably all of you again. Are you
actually classifying the disease and diagnosing it? Probably not. So the
disease is actually not well quantified… ”
He noted
that quality-of-life data is key in regards to calculating quality-adjusted
life years (QALY) for measuring medicines’ reimbursement thresholds. Thus,
quality-of-life data should be better used when licensing osteoporosis drugs,
Dr Bukhari maintained.
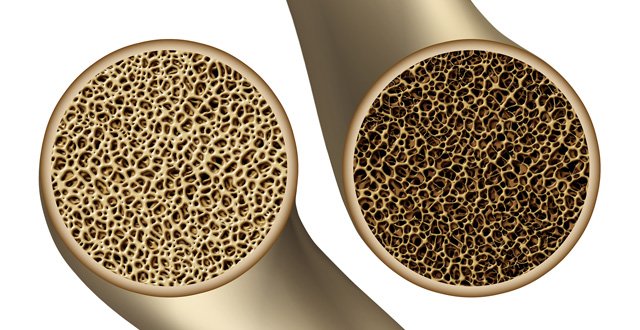
“In
osteoporosis, the problem is that in every single intervention, the outcome
measures are fracture prevention or an increase in bone mineral density. Nobody
has actually looked at patient-reported outcomes, mainly because it is quite
difficult to measure and people with the disease don’t feel ill until they’ve
had a fracture,” he commented.
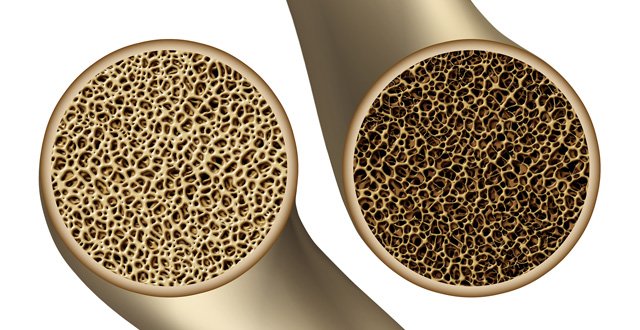
In
addition, as osteoporosis is a disease of ageing, where there will be a decline
in quality-of-life and movement typically as someone ages anyway, accurate
quality-of-life measurement can be complex, but there are measurement systems
which give more insight than what is currently used in osteoporosis.
Speaking to the Medical Independent
(MI), Dr Bukhari said that there are good treatment and
prevention options now widely available for osteoporosis, so more proactive
diagnosis and early treatment of these patients needs to happen to keep them
fit, moving and minimise fractures.
“If
they’ve got suspected osteoporosis and they’re not fractured yet, you should
really ask them is there any impairment of their mobility, what’s been
happening, are they frailer and not moving as much. The important thing really
about treating osteoporosis is lifestyle measures. So things like activity,
weight-bearing exercise, walking, doing more are always important. Once they’ve
had a fracture though, and quality-of-life goes down, it is important to
realise one fracture begets another, so you have to think about treating the disease.
Nowadays, with alendronic acid and its generic form, you can treat it fairly
easily, and not to forget the importance of vitamin D.
“It is
important to measure quality-of-life after someone has had a fracture and make
them understand that if they do exercise, it will help them as much as any
pharmacological intervention, so hopefully they will improve that way. Yes they
are scared, they have brittle bones, but it is important to get these patients
moving and keep doing weight-bearing exercise to help their bones get
stronger,” he told MI.
Dr
Bukhari also addressed ISR delegates during a satellite symposium about disease
scores in rheumatology.
“I discussed the fact that measuring RA
is easy when you are looking at swollen and tender joints but when looking at
remission, we have to take into account other features and what the patient
wants. The other features that we don’t usually measure are that we ask the
patient global [questions but] we don’t differentiate pain from inflammation
and pain from damage; it is all lumped together. So that is why it is very
difficult for us to get lots of patients into remission, as what we are asking
is a composite of several things. Therefore, remission is very difficult to do.
But on the other hand, we have five mechanisms of action, after lifestyle
advice, etc, to go for once people have active disease. And access to
healthcare and access to disease-modifying drugs early is the key to getting
patients into remission. So the distance between symptom onset and starting the
first drug is the important one and that is probably not answered in this
country, as there is a huge wait to be seen in the public sector.”




Leave a Reply
You must be logged in to post a comment.