The Irish Blood Transfusion Service Medical and Scientific Director Dr Stephen Field speaks with Pat Kelly about the challenges of maintaining blood supply during Covid and the Service’s recently published annual report.
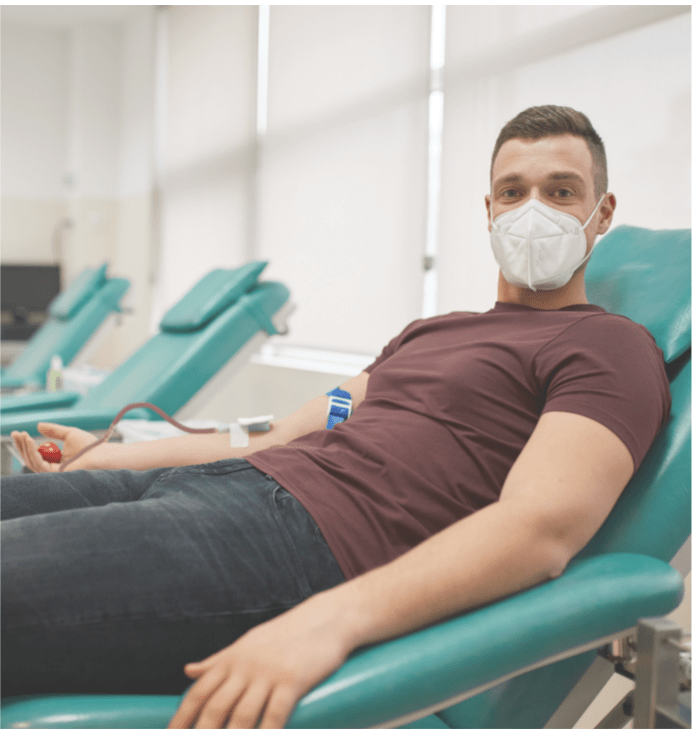
The nature of the functions of the Irish Blood Transfusion Service (IBTS) meant the impact of Covid-19 restrictions and safety measures was severe. The Service was forced to adapt at lightning speed to the rapidly evolving situation and introduced an appointments system almost overnight. However, the IBTS continued to run clinics throughout the country by implementing new work rosters, enabling hundreds of staff to work remotely, adjusting the roles of other staff, sourcing personal protective equipment, and developing guidelines to support staff, among other measures.
The Service also had to deal with hundreds of queries from concerned donors, which in itself placed inordinate strain on staff and the provision of services. Even before Covid, the IBTS had begun the consultation process for its new
strategic plan, Connections that Count:
Developing the IBTS 2021-2025, and notwithstanding changing circumstances due to the outbreak, work on this continued and was approved by its board. The re-organisation of research will enable IBTS staff to make important contributions to scientific literature in the field of transfusion medicine, including the introduction of next-generation sequencing methodology. This will provide better resolution of highly polymorphic and complex human leukocyte antigen (HLA) genes, according to the IBTS.
Dr Stephen Field, Medical and Scientific Director at the IBTS, spoke with the Medical Independent (MI) about how the Service was forced to evolve during Covid, the strategic plan, and the ongoing drive for clinical innovation. Regarding the annual report, Dr Field commented: “I think the biggest take-home message from it was we have a new Chief Executive [Ms Orla O’Brien],” he said.

Dr Stephen Field
“There was great work done by [Mr] Andrew Kelly for the previous 19 years. The Service was in a bad place when
he took the hot-seat but he has handed over the mantle of CEO to a really competent person and we are thriving under her leadership.”
‘Careful approach’
In any discussion about healthcare provision in the current climate, it is difficult to avoid the topic of how Covid has
affected care. “When Covid came about, we obviously had to take a very careful approach to protect both staff and donors at a time when we really didn’t know very much about what Covid really was,” said Dr Field.
“We also needed to cut back on the blood supply, because the hospitals had closed-up too, and so less blood was actually required. So, the first thing was that we needed to be sure we didn’t over-collect blood, because there’s nothing worse than having to discard blood on an expiry date because it’s not needed.”
It was necessary to rapidly adapt to a new system whereby all new donors had to make an appointment as the IBTS
switched its focus to existing donors during that period, said Dr Field.
“It was more difficult to process new donors in 2020 because we needed to do pre-screening; they needed to make an appointment over the phone and then come and take it up; and it’s a lot easier to do that with existing donors. We suffered as a result of that, because as our donor panel gets older, some of them will need to stop donating as they get to a certain age or get illnesses, and they need to be replaced with younger people.
The consequence is that we have a backlog on recruiting those new donors, so that’s where our emphasis is at the moment.” In spite of these difficulties, the appointments system worked well, as donors knew when they were coming to the clinic and a lot of pre-screening work was done over the telephone to eliminate anybody who was not eligible
to donate, he explained.
“Having said that, we now need to develop our software,” said Dr Field. “We have a dedicated IT system, which is a specialist proprietary blood transfusion information system, which is called a blood establishment computer system, or BECS.” The IBTS uses the eProgesa system, which is a software application that has been specifically developed to meet functional requirements of blood banks and blood transfusion centres.
“We now need to develop a portal to make the appointments system a little bit tighter and more linked-in to the
system itself. At the moment, we are just using a system we developed to see us through the crisis period.”
‘Chaotic’
He described the early “chaotic” days of the outbreak: “Firstly, we had to know a little more about the virus,” said Dr Field. “The thing that became rapidly apparent is that being a respiratory virus, it was not going to be transmitted through blood transfusion. But having said that, and knowing what we do about the emergence of viruses in the past and the havoc they can cause with transfusion, we obviously took a very careful approach.”
This involved deferring those donors who had Covid before they could donate and this all had to be reconsidered when the vaccines were rolled out, Dr Field explained. This also involved introducing a short deferral period after
a donor had been vaccinated. Another necessary measure was to introduce processes at clinics to ensure distancing and mask-wearing.
“Of course, the policies around masks changed quite a lot in those early days – were they effective, were they not effective, did people need to have them on all the time? There was a policy at one time whereby people needed to have them on during the queuing process, but when we were actually dealing with them on the donation couch, we needed to have their masks off so that we could pick up on any reactions the donor might suffer more quickly,” said Dr Field.
“Then it became apparent that it was preferred that people should wear masks all the time. We very quickly learned to pick up on people who were having adverse events relating to the donation in other ways. “All of those things needed to be worked out – we needed to look at the science, the national policy, to make sure that we were compliant.”
Whereas it was possible for some medical specialties to see patients during lockdowns and assess them via virtualcons ultations, the nature of blood donation meant that the IBTS did not have that luxury. “We needed to rely on the donors truthfully filling-in their health questionnaire, which looks at risks and so on, but they had been basically doing that for years anyway, so there was nothing new there, but we had never done telephone pre-screenings before,” Dr Field said.
When Covid came about, we obviously had to
take a very careful approach to protect both
staff and donors, at a time when we really didn’t
know very much about what Covid really was
In conjunction with the change of CEO, the new strategic plan for the IBTS was introduced following extensive consultations between different areas of the Service to identify what needs to be looked at more closely in transfusion medicine in Ireland. “It’s an evolving field,” Dr Field told MI. “In 2019, we looked at the issue of Creutzfeldt-Jakob
disease (CJD) in the context of our donors who had ever lived in the UK.
We examined all the scientific evidence and came to the conclusion that the risk is actually tiny and we could remove
that risk factor. That has also opened up the way for us to use Irish plasma in a different way. For 20 years we discarded plasma – when we produce our red cells, which is the primary part that is transfused, we had not used the plasma.
In fact, we sold it off at very cheap rates to companies that want to make controls for their blood reagent test kits, for example.” However, there is now a worldwide shortage of intravenous immunoglobulin and the rest of the world is largely dependent on supplies from the US to produce this particular fractionated medical product, explained Dr Field.
“By changing the vCJD [variant CJD] rules, we are now able to look at the plasma market once again. We have imported plasma for the past 20 years to meet the fresh frozen plasma demands in our hospitals – there is a pathogen reduction process that kills-off any viruses, etc, within the plasma,” he said.
“We have the option of sending our own plasma for that process, or we have the option of doing it ourselves using
another patented process, which is currently under procurement. So we do now have options.” The excess from the process, according to Dr Field, can now be sent to fractionation plants for the production of items such as intravenous or other immunoglobulin or albumin, for example.
This creates a revenue stream for the IBTS to allow them to look at pathogen reduction in platelets, for example,
which is a costly process. “We are hoping that we can look at the health economics of that,” said Dr Field. “Although it is expensive, it does add another layer of safety to our system, which is very safe as it is, but there is always the remote chance of something breaking through.
And if we can implement that, of course, we have to make sure that we are using taxpayers’ money appropriately.”
Sickle cell
Dr Field also touched on a plan to recruit donors of African ancestry, many of whom have lived in malaria-endemic areas of the world, in an effort to improve Rh matching of blood required for sickle cell patients. “We do need donors of African ancestry. We have an ever-growing cohort of patients in our hospitals, particularly Crumlin and St James’s Hospitals, who have sickle cell anaemia,” explained Dr Field. “The African blood group configuration for Rh is slightly different to that of Irish and Caucasian populations.
In the simplest terms, the Rh system is a complex of three different antigen types: C, D and E, and D and E are not
compatible with the normal Rh-positive Irish donors, but they are compatible with Rh-negative donors,” he said.
“So we need to collect blood [C- and E-antigens] from African donors who are Rh-positive. But the difficulty is that there is a risk of malaria,” said Dr Field. “In the UK, there are tests with malaria and we have now validated those tests here in Ireland, and we are in the last stages of getting that ready. It’s simple enough to do the tests, but we need to get the software to transfer the results from the test platform into the eProgesa system.
That requires some configuration, but we are just about ready to test that and we are hoping to get a small
group of people of African ancestry to come and give us samples so that we can test the system.”
The strategy also addresses the re-organisation of research work at the IBTS, which Dr Field has previously
stated will enable the Service’s staff to make significant contributions to the scientific literature in the field of transfusion medicine. “One per cent of our turnover is put into research and development,” he explained to MI.
“In recent years, that money has been spent externally, outside the IBTS, looking at regenerative medicines, and has been run through NUI Galway. We funded a number of regenerative medicine projects, but that funding stopped some years ago, in that those projects were complete. We then needed to re-look at our own R&D, which needed a little more facilitation and organisation.
“I’m very pleased to say that about a year ago, we appointed Dr Allison Waters as our R&D facilitator,” he continued. “She has really put the IBTS on the map in this regard and she has developed a full R&D strategy, which is available on our website and is well worth a look.” As a result, the IBTS is now examining the prospect of placing its staff into higher degree courses. This is an area the Service has always encouraged, but organising it within a department
allows all the assistance a staff member needs to put a project in place.
“We will also be working with many academic institutions and we are looking at a PhD project with our partners at St James’s and Trinity College to look at cellular therapies,” said Dr Field. “We are also looking at a joint research project with Technological University Dublin on a PhD for someone who will eventually come into the field of transfusion science. We are also hoping to try to encourage a senior registrar in haematology to come and do research Fellowship and get an MD degree, and that’s in the process of being looked at now.
If we can have trainee haematologists coming through the Service, and if we can get one of them to do a Fellowship, it may entice them into the sub-specialty of transfusion medicine, because we are very short of people in that area.”
We are in the genomics era, and we need
to start thinking about how we are going to
use our knowledge of genetic sequences…
In addition to all of these activities, the IBTS conducted a seroprevalence study on donors throughout the pandemic and the results are due to be published later in 2021. “We got some interesting results from that and it has gone in for publication,” said Dr Field.
“There was something about it splashed in one of the newspapers a few weeks ago, but we need to be quite careful in how we report our findings before they are published elsewhere.” The research is currently out on peer review, he added. However, Dr Field was able to say that a number of studies have been conducted on donors by the IBTS and the antibodies relating to Covid-19 and the results will be published shortly.
Dr Field and his team are anxiously awaiting the result of the peer review, but the process may be slower than normal, as “there is a lot of literature on Covid out there at the moment and a lot of competition for publication space”.
Sequencing
He also spoke briefly about the introduction of next-generation sequencing (NGS) methodology that has been used in the tissue typing (HLA) laboratory, which enables better matching of stem cell donors to patients who require a transplant. “It’s a very specialist field, state-ofthe-art in tissue typing, so that does guarantee better matching for our patients who need transplants for leukaemia or other haematological disorders,” said Dr Field.
“It enables the best-quality match and puts our registry on the map worldwide in terms of having the top standard in HLA typing available to us. It uses more molecular sequencing processes to get right down to the core DNA sequences of the particular HLA type, and we hope that we can expand that in time to do red-cell genotyping. That will make the matching of our donors with patients a lot more specific.
“We are in the genomics era, and we need to start thinking about how we are going to use our knowledge of
genetic sequences and how we can pick up the different blood group antigens of our donors and make sure they are
matched appropriately with our patients,” he stated. “However, we also have to be aware of the power of DNA sequencing and certain information contained in it.
What we don’t need to know, we don’t need to look at.” This would include mutations contained within blood groups.
“My term of office is coming to an end,” Dr Field told MI, whilst noting the many significant changes that have taken place within the Service in recent years. “There has been tremendous change and hopefully under a new Medical and Scientific Director, that will continue, and we can move into other areas, such as cellular therapies – I think they are the way forward for the Blood Transfusion Service, in conjunction with our transplant or haematology units treating patients with malignant disease. I believe there is a big area to be developed there.”












Leave a Reply
You must be logged in to post a comment.