An agreement was signed recently that aims to further progress cancer care and research on the island of Ireland, despite Brexit and Covid-19. CEO of Cancer Trials Ireland Ms Eibhlín Mulroe spoke with Pat Kelly about the implications of the deal
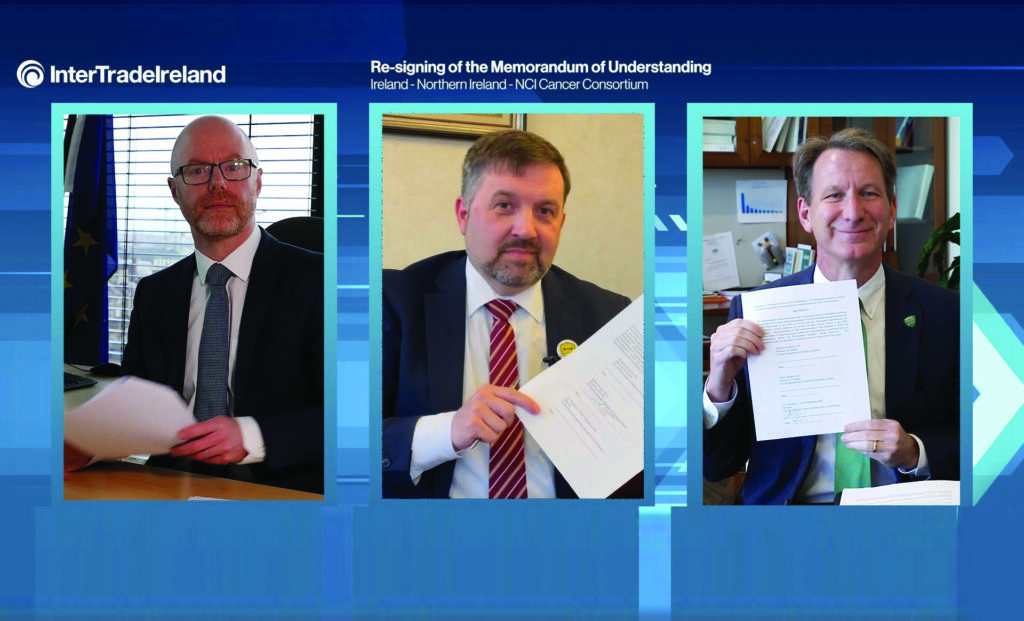
The Ireland-Northern Ireland-US National Cancer Institute (NCI) Cancer Consortium agreement was first signed in 1999, following former US President Bill Clinton’s visit to the Republic and Northern Ireland the previous year and was at that time named the All-Island Cancer Consortium. It was recently re-signed by Minister for Health Stephen Donnelly and his Northern counterpart Robin Swann, and Director of the National Cancer Institute in the US, Dr Norman Sharpless.
The objective of the agreement is to establish a robust consortium, with the aim of reducing cancer incidence and mortality on this island through cross-border and transatlantic collaborations in cancer research and education. At the re-signing on 16 March, the signatories received messages of support from Taoiseach Micheál Martin, Northern Ireland First Minister Arlene Foster and Deputy First Minister Michelle O’Neill. The current memorandum of understanding (MoU) was four years in the making.
Since its inception in 1999, the Consortium has helped to establish a robust clinical cancer trials infrastructure on both sides of the border, an All-Island Cancer Atlas, and has trained more than 500 clinicians, healthcare professionals and scientists through a number of short-stay programmes at the NCI.
An analysis of the Consortium’s work, published in 2020 in the European Journal of Cancer, showed that it had been instrumental in doubling the number of collaborative cancer research projects across Ireland and helped to significantly increase the amount of quality research published in high-impact clinical journals. Since its establishment following the Good Friday Agreement, the Consortium has enabled the recruitment of more than 35,000 people on clinical cancer trials on both sides of the border.
The re-signing event was followed by online presentations from an expert panel and patient advocates. It was explained that the three key areas the Consortium will focus on are: Improving access to cancer clinical trials; overcoming barriers to data sharing; and accelerating opportunities for education and training.
It is broadly recognised that the previous agreement had contributed significantly to boosting those patient recruitment numbers. However, at the re-signing event, Prof Mark Lawler, Chair of Translational Cancer Genomics at Queen’s University Belfast, warned that the current pandemic is doing significant damage to Irish citizens, and cancer patients specifically, and will lead to a cancer epidemic across the island of Ireland.
Implementation
Following the event, CEO of Cancer Trials Ireland Ms Eibhlín Mulroe spoke to the Medical Independent (MI) about the significant opportunities the agreement brings to cancer care on this island, as well as the challenges to full implementation of the initiatives posed by Covid-19 and Brexit.

“After the Good Friday Agreement, the late Prof Paddy Johnson [former Professor of Oncology at Queen’s University Belfast and world-leading expert in cancer research] had worked in the US in the NCI as a researcher and he came back to the North. When you train in the NCI in the US, you are among those at the top of their fields in terms of clinical trials and research and you get a taste for that,” said Ms Mulroe.
“There were other Irish doctors who trained there and what a lot of those doctors felt when they came home was that there weren’t enough options for people with cancer in Ireland in terms of trials. That can be the difference between sitting down with a patient and saying ‘you need to sort out your affairs’, or saying ‘there is a clinical trial that might give you some time with your family’, and that’s the difference. That was the driver [behind the initiative], but also to get us to work together both North and South for the benefit of cancer research.”
The MoU was re-signed every four years and as a result, a significant number of doctors and nurses had the opportunity to go to the US and sharpen their research expertise, and this created an impetus for State funding of cancer research in Ireland. “When you take a cancer patient in Donegal, for example, and they have to travel three or four hours to Galway or Dublin to get onto a clinical trial, maybe every week, some patients just decide that they don’t want to do that,” said Ms Mulroe.
“So it would be much easier for them to go to Altnagelvin Area Hospital, for example, and the same is true for patients in Fermanagh or Tyrone, for instance.
“Also, we want to be able to offer the same trials in Dublin as we do in Belfast, but one of the things that this MoU really captures is that you cannot work on clinical trials in a small island like ours on your own – you need to work globally,” she continued. “The NCI opened doors to allow us to do that, so patients in the US and Ireland were being recruited onto the same trials with the same protocols.”
Many of the pharmacists in our hospitals will say that our funding through the HRB and the Irish Cancer Society has enabled them to work on clinical trials
One of the ways to develop these links is to explore more training opportunities for doctors, nurses and translational researchers and for governments on both sides of the border to examine ways to enhance activity in research and trials in Ireland, “and that’s all happening now and it’s very exciting,” said Ms Mulroe. “It’s a bit like the Good Friday Agreement, in that all the right people were in the right place at the right time, albeit in a different context and at a much smaller level.”
Irish physicians who work with the NCI in the US and return to Ireland bring with them not only greater expertise, but also a network. One example is Prof Austin Duffy, University College Dublin Associate Clinical Professor, and Consultant Medical Oncologist, Mater Misericordiae University Hospital.
“He has run a parallel trial with the NCI in the past two years in liver cancer,” Ms Mulroe explained. “He mirrored the protocols and patient population and it has worked really well. We see that as a pilot in terms of how we can do more.”
Brexit
Despite the well-publicised concerns over the impact of Brexit on cross-border healthcare collaborations, Ms Mulroe was positive about the Consortium’s ability to overcome any such challenges. “Brexit has not affected any of this as yet,” she told MI.
“Cancer Trials Ireland is a not-for-profit collaborative group in the Republic, but we open and run trials all over Europe. We sponsor clinical trials; if you don’t work in clinical trials, the word ‘sponsor’ suggests that we fund it, but when you are the sponsor of a clinical trial, it basically means you are the one that the regulator holds accountable for the entire running of the trial, from the protocol development, recruitment of patients, data management, auditing – you are responsible for all of that.
“Because we are in Europe, it has been attractive for global not-for-profit academic groups to come to us. ANZUP [Australian and New Zealand Urogenital and Prostate Cancer Trials Group] is a really good example of that. We have opened trials with them; they are not allowed to be the European sponsor, so they align themselves with groups like us,” she continued.
“We also open trials in the UK, so it’s not just about Belfast; we have trials open in London, Glasgow, and Edinburgh, for example. Even with Brexit, we have managed to navigate trials in the North and in the UK, so within the health research community in the wider UK, there is a real desire to continue to do research with Europeans,” said Ms Mulroe.
“Even their regulator, the MHRA, wants to continue to align with the EMA and hopefully that will continue because the relationship between Ireland and the UK from a research perspective is really important.
“I have personally learned so much from them in the context of patient involvement in research. I think the UK has led the way in that space and it’s something that we also hold very dear. It’s important for people in Northern Ireland to hear that too, that no matter what persuasion you are, cancer is cancer and there are no borders when it comes to this disease.”
When running a clinical trial, it is vital to recruit the appropriate numbers, she explained. “For example, with pancreatic cancer, you’re not going to get 1,200 patients in a site in Dublin, for instance. You need to have a number of different hospitals involved and that’s why you need to go beyond your country’s borders and work together. It’s difficult when you are a not-for-profit organisation, but we have done it.”
When Irish doctors and nurses go to a hospital that is NCI-funded, they gain access to a range of resources that are not available to them in Ireland, including being part of a team that works exclusively on clinical trials. Ms Mulroe recalled being taken aback when visiting an NCI facility that was a bespoke hospital dedicated to clinical trials and described it as “an amazing vision for the future in Ireland”.
“When you come back from a facility like that to somewhere like Beaumont or Cork or Galway [hospitals], you simply don’t have the same resources. If it wasn’t for the HRB [Health Research Board] and Irish Cancer Society support for Cancer Trials Ireland, we wouldn’t be here and we wouldn’t be able to fund those hospitals to employ nurses, data managers and pharmacists to run the trials,” she added.
Ms Mulroe continued: “If you are running a clinical trial with a drug, that just can’t be done without a clinical pharmacist, so they are crucial. We have had trials paused simply because we did not have a pharmacist on-site to mix the drug and prepare the drug for the trial,” she said. “When you are preparing a drug for a trial, you can’t just use an off-the-shelf product. It needs to be labelled appropriately as an investigational product, even if it is standard of care. There is a whole process around that and pharmacists are really key to that.
“Many of the pharmacists in our hospitals will say that our funding through the HRB and the Irish Cancer Society has enabled them to work on clinical trials. But when you have worked in other countries – we do okay [in Ireland], but we could do better – you see that the health services fund people to work in clinical trials, whereas here, we rely on our health research funder, and that’s not good enough. We do have to look at the HSE and NCCP [National Cancer Control Programme] to see how they might structure jobs within the health service so that there are people who work exclusively on research and trials. That’s a big conversation – we are getting somewhere with it and it’s great that the HSE has finally appointed someone who is in charge of research, but we could probably do better.”
Ms Mulroe also spoke about the importance of clinical pharmacists on trials in the context of potential drug-drug interactions. “In terms of adverse events in trials, we have a whole pharmacovigilance department and some of the people working there are pharmacists. Every adverse event has to be reported within 24 hours; we have a medical oversight team that reviews all of them, but it’s massively important to have a good pharmacist to ensure safety in your trial.”
Covid-19 and cancer
Ms Mulroe went on to speak about the serious consequences of Covid-19 on cancer care in Ireland in terms of missed diagnoses and treatment. “Dr Sharpless has predicted a 10-year mortality increase as a result of Covid in the US and it’s going to be the same here,” she told MI. “People are coming to the clinics later, their cancer has progressed further than it should have, people were not being screened, so there will be an obvious knock-on effect. We are bracing ourselves for that – we have written to the Minister for Health and asked for a meeting on this.
“The Irish Cancer Society has co-signed the letter. We want to reframe the cancer strategy because to be honest, it is sitting on a shelf. It was published in 2017 and very little has happened to the strategy since then. Particularly from a research perspective, it lacks an implementation piece and we want to look at that with a Covid lens, because we are going to have to change focus and we will have to be ready with clinical trials too. There are going to have to be some hard conversations had with people with cancer and we want to be able to say to them, ‘we have a trial that might be able to help you.’”
Cancer Trials Ireland’s accrual numbers represent the numbers of patients recruited onto trials. The level of accruals is now 40 per cent below normal. “However, the pharmaceutical-sponsored trials are actually up compared to last year in terms of the numbers of patients on trials,” said Ms Mulroe. “They would pay the sites more to do the trials so there could be a financial aspect, but in fairness, there are some very good pharmaceutical treatments out there and people want to get them to their patients.
“We have to work out how we are going to be able to enhance activity over the next five years so that we are ready for that [cancer backlog],” she explained. “Some have called it a potential tsunami of cancer patients over the next five years. A lot of health issues will result from Covid, such as mental health and cardiology, but cancer care will of course also be affected and we have to be ready for that.”
People should ensure that they still contact their GP if they are worried and should actively seek screening, she stressed. “From my point of view, I would look at people who don’t have private healthcare and wonder if they have the same options – I don’t think they do. You may be seen more quickly if you have private health insurance
than if you don’t and that’s not fair. We really need to challenge that and that’s one of the reasons why we want to talk to the Minister and look at a strategy for cancer for people after Covid.”
The future
In terms of her hopes for the future of the Consortium, Ms Mulroe said: “I want to see that patient in Donegal getting into their car, going to Altnagelvin [Hospital] and getting on a trial, and vice-versa. I want to see doctors and nurses from both sides of the border sitting together and planning trials – that’s already happening, but we need to see more of that.
Dr [Norman] Sharpless has predicted a 10-year mortality increase as a result of Covid in the US and it’s going to be the same here
“I also want to see that group discussing trials with clinicians in Washington or New York, for example,” she continued. “We have really good examples of that, but we want to do more. I want to see what I experienced in Washington replicated in Ireland; we want to see bespoke clinical trial facilities for people with cancer in our sites in Ireland. We can’t do everything everywhere, but what we can do is take particular sites with particular expertise in certain disease areas that we could turn into centres of excellence for clinical trials.”
Ms Mulroe was particularly struck by the efforts of Irish champion jockey Pat Smullen, who passed away from pancreatic cancer in September last year. He approached Cancer Trials Ireland and was shocked to learn that the charity was unable to open a trial on pancreatic cancer at that time, as for a trial to be opened, it is necessary for a charity to demonstrate an ability to fund the trial for its full duration.
“He thought that was ridiculous,” said Ms Mulroe. “A trial wasn’t going to help him, but for the greater good, he reached out to the horseracing community and raised €2.5 million in one weekend and even now, there are still jockeys, staff, and other people involved in horseracing who still send us cheques and fund horses to run for us… he did that for everybody else and it does make a difference, because we now have three trials – one has opened, another is in the offing. None of them will find a cure in the morning, but they will help and perhaps give some time to people and provide some answers for our researchers.”
Ms Mulroe explained that her ambitions include enrolling at least 6 per cent of cancer patients onto trials, and that every cancer patient should be asked if they would be interested in participating in a clinical trial. “Every patient should have that opportunity in Ireland, but they don’t,” she told MI. “Sometimes you don’t even need to be on a clinical trial; there are good treatments for cancer and there is hope for those people who receive a diagnosis, thanks to the research that has already been done. But for those people for whom there is little hope, we want to do more.”
Cancer Trials Ireland is to host an inaugural Cancer Retreat on Friday 21 May from 9am to 4pm. The day-long event will address the next five years in Irish cancer clinical trials, and features presentations and panel discussions from Professors Ray McDermott (Clinical Lead, Cancer Trials Ireland) and Seamus O’Reilly (Vice-Clinical Lead, Cancer Trials Ireland). Panellists and participants will explore funding trials, recruiting patients, an all-island approach to research and care, trial selection processes for Disease-Specific Sub-Groups, and trial logistics. To view the Retreat programme and to register free of charge visit www.cancertrials.ie













Leave a Reply
You must be logged in to post a comment.