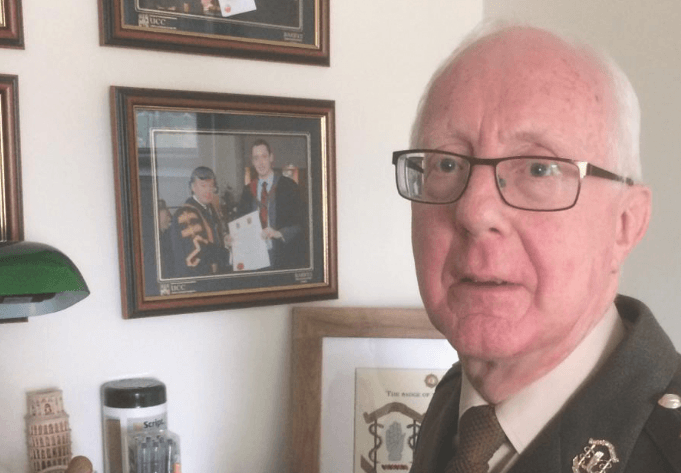
Colonel Dr Gerald Kerr, Outgoing Director of the Defence Forces’ Medical Branch, spoke to the Medical Independent about his more than 30 years of service in military medicine — an exhilarating journey with many challenges and opportunities
In 1986, Colonel Dr Gerald Kerr began life as a military medical officer. It was seen as the road less travelled and even “a bit of a gamble”.
“In retrospect, it was a most interesting and rewarding experience. After 33 years’ service in uniform, I would not exchange even 10 minutes of it for any other medical service,” Dr Kerr told the Medical Independent (MI).
Military life, when he joined, was “largely restricted to garrisons, which were surrounded by secure and high walls”. The public generally had little knowledge of what members did all day behind these walls. “And such lack of knowledge was just one step away from the assumption that they did nothing,” according to Dr Kerr.
“A similar perception could be found in the medical community about the practice of medicine in the Defence Forces. This was compounded by the widespread view that Defence Forces personnel were ‘all young and healthy’.
“Consequently, those who opted to devote their lives to the medical care of military personnel were suspected of seeking ‘an easy life’ with minimal challenges. This was a commonly held view among medical peers and colleagues at the time. The reality, however, was totally different. Military medical life has proven to be interesting, varied, challenging and rewarding.”
Variety
The variety of challenges encountered reflects the diversity of medical practice in the military environment. Primary care in the military produces the same type of challenges as in any general practice, but assumes an increased level of complexity in austere environments overseas where resources are limited, according to Dr Kerr.
“Apart from the uniqueness of the military medicine consultation, the daily tasking can bring additional variety. The medical officer (MO) today could be engaged in providing ‘sick parade’ services, tomorrow he/she may be called upon to provide medical cover ‘in the field’ on an exercise in the Galtees, or to an artillery shoot in the Glen of Imaal.
“The following day, the MO could be required to participate in a medical board charged with adjudicating on the fitness or otherwise of an individual for further service. Other tasks can include providing medical briefings to operationally active personnel or carrying out reviews of those on long-term sick-leave. These are just some of the many tasks which an MO is required to undertake. Boredom is not a state associated with military medical service!
“Our involvement with the Partnership for Peace alliance brings opportunities for military medical courses abroad, including in Germany, Switzerland and the United Kingdom. In addition, service overseas adds a further dimension of variety to an MO’s job specification. This includes deployments with the United Nations, or on EU Missions.”
Dr Kerr completed his training in general practice before joining the Defence Forces. It was “a great privilege to utilise those skills” as Battalion Medical Officer in the 28th Infantry Battalion in Donegal for 10 years. During this time, he twice served in South Lebanon with the United Nations Interim Force in Lebanon (UNIFIL).
Subsequently, Dr Kerr served with a Reserve Unit in the Southern Brigade, where he was strongly involved in first aid and Advanced Trauma and Life Support (ATLS) instruction.
“My educational opportunities within the military environment were not confined to ATLS. I was facilitated in undergoing various courses and receiving qualifications in occupational medicine, tropical medicine, sports and exercise medicine, as well as orthopaedic medicine.
“As a result of the latter two areas, I travelled to the International Military Sports Council (CISM) World Military Games in Hyderabad, India, in 2007 and to Rio de Janeiro, Brazil, in 2011 to provide sports medicine ‘cover’ to the Defence Forces athletes attending these Games.”
Training policy
In 2010, Dr Kerr was appointed Director of the Medical Branch, with a key area of responsibility being formulation of policy on medical education and training.
“I adopted a three-pronged approach to this area, beginning with the roll-out of the Military First Response Course for all personnel,” outlined Dr Kerr.
“This course was devised with the assistance of the Academy of Emergency Care in Cork and among others, the late Mr Paul Allen. The objective was to give all personnel the necessary skills to cope with the first 10 minutes of either a medical or trauma-related emergency.
“The second educational initiative was designed to expand the capacities and capabilities of medical personnel of the Defence Forces. This gave rise to the level 7 university qualification (Diploma in Military Medical Care), which incorporates the Emergency Medical Technician Practitioner qualification, as well as providing the graduates with all the skills required by medical personnel in their occupational or garrison role. Such skills included audiometry, spirometry, phlebotomy, vision-testing, administration of vaccines, etc.
“The third element of the educational policy was aimed at medical practitioners. It related to the establishment of the specialty of Military Medicine and the associated accredited training programme.”
On this latter development, Dr Kerr said there was firstly a need to recognise the unique nature of the practice of medicine in a military environment. Secondly, medical training within the military prior to accreditation of the training programme was ‘ad hoc’.
“Such a cavalier attitude to the medical care of members of the Defence Forces was not acceptable in the long term, especially when considering the Medical Council’s desire to ensure that patients, where possible, came under the care of specialists.
“Thirdly, there was a need to establish that those best equipped to deal with medical issues in the military environment were those who were part of that environment, who fully understood it in all its aspects and who could interpret medical issues and problems in light of their own experience in that environment.
“Fourthly, there was a need to make military medical service relevant and something of value when the medical officer decided to return to civilian practice. Thus, the link between the Faculty of Military Medicine and the ICGP, and the fact that the successful graduates of the training programme will have dual entry onto the specialist division in Military Medicine and General Practice.”
Asked if the training programme has solved MO recruitment difficulties, which have plagued the Defence Forces for years, Dr Kerr said “it is early days yet”.
“The first trainees only commenced their two-year initial specialist training in 2017, and this year marks their transition into the three-year higher specialist training element of the programme. It is indeed hoped that Military Medicine and the associated training programme will provide a steady flow of medical officers to enable the Defence Forces fulfil its commitments both at home and abroad. This outcome will take many years to come to fruition.
“But as an indication that things are heading in the right direction, the most recent intake of so-called ‘direct entry’ medical officers were offered contracts of services for three years only in order to ‘make room’ for the entry into full-time service of the newly-qualified specialists. The situation remains dynamic, and changes to the terms and conditions of service will reflect service needs and requirements. The most recent change to be introduced was the extension of the age limit of applicants for the training scheme to 40 years of age.”
To date, the application process has been over-subscribed every year.
“The scheme is a small one, involving only two trainees per year. However, like many new and not-so-new training schemes, the Military Medicine training scheme has experienced some teething problems. The selected candidates for a July 2019 commencement have withdrawn from the scheme, and there was insufficient time to embark on a new recruitment campaign. Thus, 2019 will see an ‘operational pause’ to the training scheme, but plans are already in place to re-enter the ‘marketplace’ in 2020.”
Mental health services
Since the closure of military hospitals, personnel have become largely dependent on the civilian health system for secondary care. The national media has publicised delayed access to psychiatry services for military personnel.
“As the public system has come under increasing pressure, waiting lists have increased. One specialist area which has been particularly badly affected is that of psychiatry,” confirmed Dr Kerr. “The nature of military service, both at home and abroad, can be very stressful and it is not therefore surprising to learn that the various manifestations and complications of stress can be commonly found at sick parade.
“While most of these issues can be successfully treated at the primary care level, the minority require specialist intervention. Within the civilian health service, there is little if any difficulty in accessing emergency care, but there is a problem with ongoing non-emergency care.”
The loss of a dedicated and uniformed military psychiatrist has amplified this problem. “While a recent campaign to recruit a military psychiatrist in the rank of lieutenant colonel has met with no success, there is currently an intensive recruitment campaign to engage a full-time civilian psychiatrist for the Defence Forces. Being eligible for a higher rate of pay than a commissioned lieutenant colonel, it is hoped that this campaign will be more successful.”
Regarding psychological services, the Defence Forces has recently increased the number of full-time clinical psychologists engaged, and this service has been augmented as required by a Reserve clinical psychologist.
“In addition, the role of the personnel support services should not be underestimated in facilitating education on and prevention of the manifestations of stress, thereby facilitating early identification and onward referral.”
Meanwhile, Dr Kerr emphasises that the fundamental ethics of medical practice apply to military doctors.
“There has in the past been a lack of understanding among some within the military command structure of the ethical code with which medical officers must comply,” he explains.
“Failure to comply with the ethical code and the associated guidance provided by the Medical Council could result in a medical officer being struck-off the medical register… In recent years, as Director, Medical Branch, I have addressed this issue during junior and senior officer career courses.
“Interference with clinical impartiality and autonomy is not acceptable and cannot be tolerated. The Medical Council, in the opening paragraphs of the current Guide to Professional Conduct and Ethics for Registered Medical Practitioners, emphasises that ‘medical care must not be used as a tool of the State. As a doctor, you must be free to make judgements about your patients’ clinical needs and to give appropriate treatment without political pressure.’”
Anti-malarial drugs
Over recent years, a controversial aspect of healthcare in the Defence Forces has been prescription of the anti-malarial Lariam (mefloquine) to some personnel on overseas missions. Legal actions have been initiated, alleging enduring adverse effects associated with the medication.
According to Dr Kerr, it is widely accepted that malaria is a serious illness that can be fatal.
“Therefore, it is the policy of the Defence Forces to reduce to the minimum the risk of personnel becoming infected with malaria, especially when deploying to sub-Saharan Africa, where the most dangerous form of malaria is rampant.”
There are two types of preventative medication, one taken daily and the other weekly. The medication taken as a weekly regimen (Lariam) has two positive consequences of value in the military environment, according to Dr Kerr.
“Compared to a medication which must be taken every day, it presents six less opportunities in seven days to miss or forget a dose. In the military context, this is advantageous, as particularly in an operationally volatile deployment, predictability and freedom of activity cannot be guaranteed.
“This means that there is no guarantee that the patient will be able to take the required medication at the appropriate time. Hostile combat forces do not give advance notice of the time of their assault, nor do they permit a ‘time-out’ to opposing forces to allow them to take their anti-malaria medication.”
Secondly, a medication which has a daily dosing regimen loses its activity seven times more rapidly than one taken weekly. Consequently, the omission of a single dose of a daily medication renders the patient immediately vulnerable, whereas in the case of a weekly medication, there is a far slower decline in efficacy when a dose is missed, which means the patient has some ongoing protection.
“Thus, to maximise the protective potential for its personnel, the Defence Forces routinely uses a weekly rather than a daily malaria preventative medication when deploying to an operationally-volatile environment.
“Regarding Lariam itself, there are contraindications to its use in the first place, and even those who do not have any contraindications may illustrate a sensitivity to its use. The Defence Forces, unlike certain other international military forces, has always carried out individual medical assessments of fitness for deployment, including suitability for indicated vaccinations and medications.
“Those who have contraindications to Lariam are not permitted to deploy on a mission where Lariam is required. In order to detect those who have a sensitivity to Lariam, the medication is commenced three-to-four weeks in advance of deployment so that the sensitivity will become apparent while still in Ireland.”
Dr Kerr said the media has reported accounts of horrific personal experiences that have been attributed to Lariam.
“The problem is, however, that several other possible causes of the horrific symptoms often coexist, and the challenge is to differentiate between a confounder and a causative agent.”
Dr Kerr added that medical bodies such as the World Health Organisation and Centres for Disease Control and Prevention endorse the use of Lariam in the prevention of malaria, while the drug has never had its license withdrawn because of concerns related to its safety.
He said Lariam remains “a valid choice for malaria chemoprophylaxis with relevance for Military Medicine”.
Medical standards
Looking to the future, Dr Kerr encourages continued growth of the MO personnel strength to ensure universal access to comprehensive surveillance health.
“At one time in the recent past, the number of medical officers had fallen to 16, but now the strength has reached the low 20s.”
He said reform of the medical reserve holds huge potential for increasing both capacity and capability of the Defence Forces medical services.
Dr Kerr further noted that the amount of dental morbidity on overseas deployment is “quite striking” and this finding is not confined to Defence Forces personnel, as evidenced from morbidity returns from international missions.
“The number of commissioned dental officers has remained static at a very low level, and while the result of the internal review of dental services is awaited, dental morbidity, even among those screened prior to deployment, will continue to put pressure on the dental element of the Medical Corps.”
The increasing exposure given to mental health issues is to be welcomed, but comes with additional demands for resource-rich interventions, added Dr Kerr.
“I would like to see a change to the medical standards applied to contract renewal for Defence Forces personnel which are, I believe, excessively high. The current standard has been determined by factors not exclusively medical, but the Medical Corps is, wrongly, held to be responsible. One of the consequences has been that personnel are discouraged from presenting with their medical problems for fear that it will prevent renewal of their contract.”
Dr Kerr also advocates for increased understanding and acceptance of the ethical constraints under which all medical personnel are required to work. “This would contribute to a better understanding of the medical services, as well as those who provide them, to the benefit of all who avail of them.”
Overall, the military doctor can look back with much pride on a number of innovations under his watch, including advances in Irish military paramedicine.
After several years of discussions and preparations, he was particularly pleased to see a Defence Forces ambulance, stocked and crewed to National Ambulance Service (NAS) standards, assisting the NAS as part of the emergency medical response on a regular basis.
“Rotation of Defence Forces paramedics and advanced paramedics from around the country onto this ambulance service ensure that all practitioners can achieve the required clinical exposures on an annual basis,” he said.
“In addition, the Defence Forces Medical Corps is seen to contribute to the wider medical needs of the community.”













Leave a Reply
You must be logged in to post a comment.