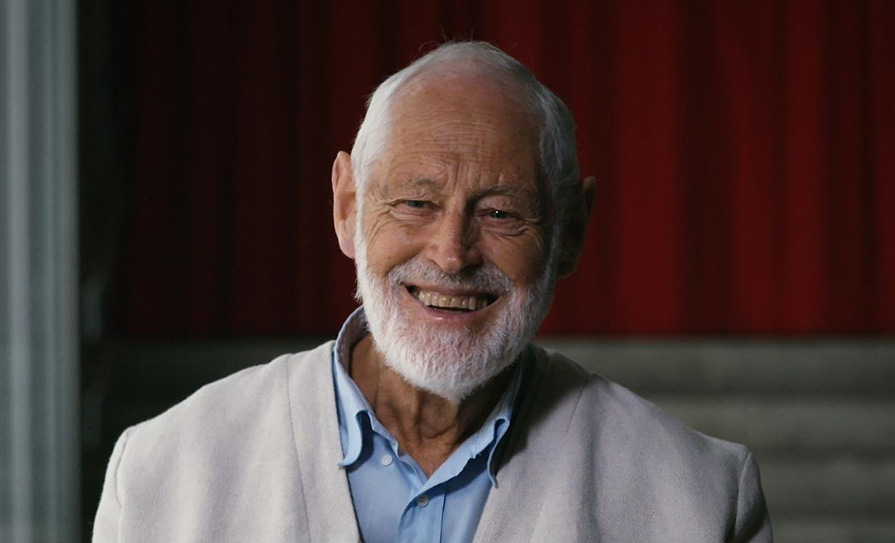
Mr Neil Kidd explains the benefits of open disclosure for the health service, medical profession, and patients
The medical profession is not exempt from human error, and when it occurs, the consequences can be devastating for both the patient and the medical team. As a medical negligence solicitor I see first-hand how medical errors can be life-changing for clients and their families. It is an extremely challenging time in any person’s life when they suffer a serious injury. This is compounded if that injury was due to negligence and ought never to have happened in the first place. A subsequent failure to provide a full explanation of how the damage occurred will invariably have an adverse effect on the patient’s outlook of what they have suffered. From the patient’s point of view, it is bad enough to feel let down by the treatment they have received without adding a feeling that information is being withheld. Most clients I come into contact with want to know why their injury occurred and that what has happened to them will not happen again. Financial compensation is often not at the forefront of clients’ minds and pales in comparison to the natural human desire for answers and reassurances that lessons will be learned.
Open disclosure
The HSE defines open disclosure as “an open, consistent approach to communicating with service users when things go wrong in healthcare”. The HSE guidance also states that “this includes expressing regret for what has happened, keeping the patient informed, providing feedback on investigations and the steps taken to prevent a recurrence of the adverse event”.
There is currently no mandatory statutory requirement for a medical practitioner to be candid with patients. The current legal framework (The Civil Liability (Amendment) Act 2017) confirms that the disclosure of a patient safety incident is voluntary and is ultimately at the discretion of the health services provider, giving higher priority to doctor/practitioner’s decision than to a patient’s right to know that they have suffered an adverse event.
The voluntary nature of open disclosure in the 2017 Act may be superseded by the Patient Safety Bill 2018, should that ultimately be signed into law. The crucial difference between this Bill and the 2017 Act relates to the mandatory versus voluntary nature of disclosure.
The importance of open disclosure
The concept of open disclosure seems to be gaining traction amongst the medical community. Open disclosure has far-reaching outcomes, which positively affect both patients and healthcare professionals.
Reduction in litigation
A culture of secrecy has often shrouded medical errors due to a fear of litigation. However, this has had the opposite effect. Unable to secure answers, patients turn to the legal profession for guidance resulting in the drawn-out, adversarial process of litigation. It is my experience that most people are willing to accept that mistakes can be made and that no one is perfect. What they cannot accept is a lack of honesty about what has occurred. Secrecy cultivates feelings of anger, frustration, confusion, vulnerability and mistrust. It is often these feelings that ignite a desire for injured patients to commence legal proceedings. In contrast, open disclosure, including an explanation on what went wrong, can preserve the relationship and promote trust between the medical practitioner and the patient, reducing the volume of litigation and, therefore, insurance premiums.
Reduction in legal costs
Where a full explanation has been given to an injured patient, even where litigation does subsequently occur, it will be more focused on the actual issues at play. Where a patient has been left in the dark as to how and why they suffered an injury, they will need, through their solicitor and independent medical experts, to conduct a lengthy review of all aspects of the care provided. The litigation then becomes much more contentious and protracted, leading to increased costs for all parties.
Better treatment for the patient
Open disclosure permits the patient to be satisfied that he/she has obtained the necessary treatments to rectify the medical error which has occurred (if possible), be that from their initial treating doctor or elsewhere.
Improvement in overall patient care
This benefit is best summarised by Minister for Health Simon Harris: “Creating a culture of open disclosure and learning from the things that go wrong is the bedrock of making services safer.” Open disclosure provides valuable information, which can minimise the likelihood of a medical error from happening again. It also results in an increase in patient safety incident reports about where mistakes have occurred and how to avoid repeating them. Being satisfied that lessons have been learned is also of huge importance to an injured patient.
Conclusion
It is important to stress that the importance of compensation is not being denied. Compensation for medical injuries provides those injured with recompense for any pain and expense they have suffered and with the necessary resources to live their lives to the fullest of their abilities where they have suffered a serious injury. However, the importance of an explanation/open disclosure cannot be over-stated. Compensation only has the ability to benefit the injured party and disadvantage the service providers. Open disclosure provides countless benefits to both the healthcare community and the patients.
Finally, regardless of the tangible benefits discussed above, when somebody suffers an adverse outcome from a medical procedure, being given an explanation for what happened should be an absolute right and not a privilege.
Neil Kidd is a partner in Augustus Cullen Law Solicitors’ medical negligence department. He has extensive experience in catastrophic birth injury and spinal injury cases together with matters arising out of the misdiagnosis of cancer, negligent surgical procedures, nerve damage, orthopaedic injuries and gynaecological injuries.











Leave a Reply
You must be logged in to post a comment.