It is estimated that currently, about 40 million people are living with HIV worldwide. HIV has caused more than 30 million deaths since the early 1980s – nearly one million people annually on average. While infection rates have slowed in some countries, particularly those across Sub-Saharan Africa, it is still a leading cause of death.
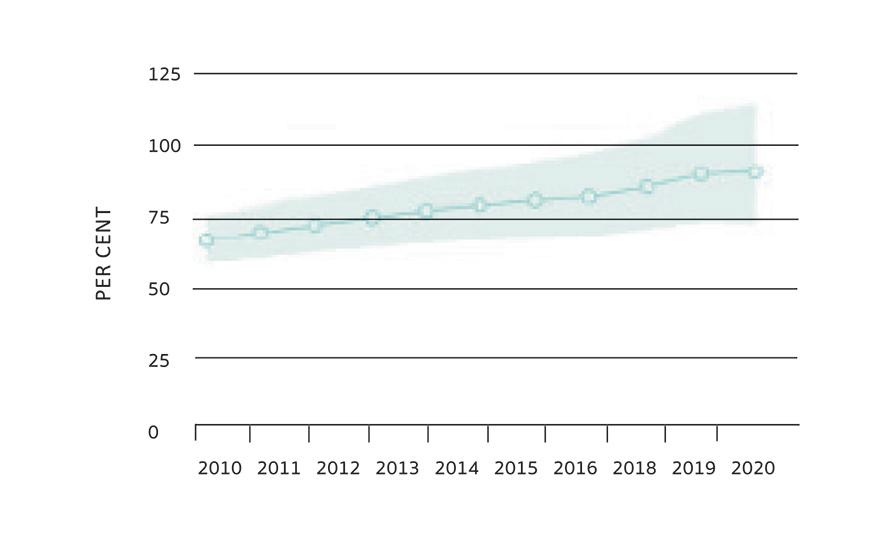
Figure 1: The coverage of people in Ireland receiving ART between 2010-2020 (UNAIDS)
Antiretroviral therapy
The availability of life-long antiretroviral therapy (ART) has transformed HIV from being severely debilitating and likely fatal, to a manageable chronic health condition. Globally, 1.2 million deaths were avoided in 2016 as a result of ART. Without ART, it is estimated that twice as many people would have died from HIV/AIDS.
The population of people receiving ART globally has increased significantly: In 2005, only two million people in the world were taking ART. By 2018, this had increased substantially to 23 million. However, 23 million is still just a proportion – 61 per cent – of all people with HIV. To increase treatment coverage, access to testing needs to be improved. Studies suggest that acute HIV infection may have a huge role in the spread of the disease, with predictions estimating that it is responsible for between 10 and 50 per cent of new cases.
People with HIV who do not have detectable plasma loads cannot transmit the virus to others (also known as U=U, undetectable equals untransmittable); however, the diagnosis needs to be made and treatment needs to be commenced in order to make this a reality. The lack of insight or awareness into many cases of positive HIV status presents a substantial barrier to the aim of achieving no further spread of infection or deaths. Among people with HIV who do know their status, stigmatisation both from others (usually coming from fear about HIV), and internalised stigma leads to a decrease in engagement with care, treatment and prevention services.
HIV infection
The compromised immune system in HIV is due to a loss of CD4 T-cells, which is the target cell of the HIV virus. HIV enters the cell after binding to the CD4 receptor (via HIV envelope protein gp120), and to a co-receptor, CC-chemokine receptor 5 (CCR5). This leads to a fusion of the virus with the CD4 cell, permitting the eventual production of new virus particles. HIV uses the host cell synthesis machinery to replicate, and also integrates a copy of its own RNA genome into the infected host cell chromosome, making it a very persistent and challenging virus to eradicate fully. Health complications and mortality rates increase as the amount of these CD4 T-cells decline.
Before publication in 2015 of the START study, which followed 4,685 patients with HIV in 35 countries for an average of three years, it was common practice to delay the initiation of ART in asymptomatic patients until their CD4 cell count dropped below a certain threshold, whereas now, ART is started as soon as possible. The immediate initiation of ART was found by the START study to be more effective, with a 72 per cent relative reduction in serious AIDS-related events in the immediate-initiation group.
HIV treatment in Ireland is free and available to everyone. In 2017, the HSE published a position statement which recommends that all individuals living with HIV attending HIV services in Ireland are offered ART as soon as possible and informed of the benefits of ART in improving their personal health and reducing HIV infectiousness (Treatment as Prevention; TasP).
ART therapy mechanisms
Multiple mechanisms along the route of HIV infection of host cells have been targeted for drug treatment. The following drug classes have been developed:
- Entry inhibitors (which prevent viral binding of the viral gp120 protein to the host cell receptor, and viral binding of the virus to the CCR5 receptor).
- Nucleoside and non-nucleoside reverse transcriptase inhibitors (preventing transcription of viral RNA into DNA).
- Integrase inhibitors (preventing integration of the viral genome into the host’s genome).
- Protease inhibitors (preventing cleavage of viral polyproteins into functional units).
Severe adverse events have been observed for several classes of these drugs, some of which have been attributed to population genetic variation. It is important that HIV ART is tailored to the individual, and in some situations, the population also.
Clinical and epidemiological studies have noted that differences in the course of HIV infection are not completely explained by variables such as age and comorbidities. One of the now most-recognised contributors to resistance against HIV infection is related to the CCR5 receptor: People who carry two loss-of-function variants in the gene encoding this are resistant to HIV infection. This was first identified in a group of men who have sex with men (MSM) who, despite multiple exposures to the virus, did not become infected. These people all carried a deletion in the CCR5 gene (the CCR5Δ32 allele) that produced a non-functional CCR5 receptor.
Interestingly, it is bone marrow transplants between CCR5Δ32 donors and recipients with HIV infection that have resulted in the only three confirmed cases of long-term HIV cure. This genetic variant is seen in about 10 per cent of Europeans and not observed in any significant frequency in other continental populations. However, as in many diseases, high-income populations have been disproportionately studied: As genetic studies expand to include more diverse populations, additional discoveries in the genome may be expected.
HIV in Ireland
It is estimated that over 8,000 people are living with HIV in Ireland. About 15 per cent of people infected here with HIV are unaware of their infection status. In the years 2003-to-2015, about 300-to-400 people were testing positive each year, but from 2015 numbers rose, to 400-to-500 cases annually until the Covid-19 pandemic.
The rate of first-time HIV diagnoses (3.4 per 100,000 population) decreased by 16 per cent in 2022 compared to 2019 and is lower than the rates between 2012 and 2018 (Health Protection Surveillance Centre (HPSC)). Over 50 per cent of cases of HIV in Ireland are among MSM (58 per cent in 2022), with the other 50 per cent among heterosexual men and women, and intravenous drug users.
However, overall HIV diagnoses in Ireland, largely among non-native populations, have increased in the last few years, and are now among the highest in Europe. A total of 884 HIV diagnoses were made in Ireland in 2022, an increase of 68 per cent compared to 2019.
Voluntary community-based HIV testing (VCBT) services are offered for free in a variety of non-clinical community settings, including mobile and outreach, for example; NGOs, including, ie, AIDSWest, GOSHH, the Sexual Health Centre Cork; and via the KnowNow programme in Galway, Limerick, Cork, and Dublin. These services target people most at risk of HIV infection, with the aim of improving detection and therefore early treatment initiation, and decreasing onward transmission.
The HPSC started monitoring VCBT (collating anonymised data from January 2017 onwards) to identify any trends in infection rates and to determine if target groups are being effectively reached in the community. The most recent report from 2022 recorded 3,142 community-based HIV tests carried out by five partner organisations, representing a two-fold increase compared to 2021 (n=1,433).
Of those tested, 20 individuals had reactive test results (five already known), giving an overall HIV test reactivity rate of 0.6 per cent, similar to 2021 (0.7 per cent). In terms of demographic breakdown, the highest rate was observed in migrants from countries with high HIV prevalence, and second-highest in MSM.
The National HSE home STI testing programme provides a home testing service for STIs and HIV, and the MPOWER programme within HIV Ireland has a HIV self-testing programme for gbMSM since 2020.
Post-exposure prophylaxis
For people who may have been exposed to HIV infection risk, post-exposure prophylaxis (PEP) is available in Ireland: It can be started for up to 72 hours after HIV exposure, which reduces the chance of HIV infection. PEP is available for free from genitourinary medicine/STI clinics and emergency departments (although there may be a charge for using the emergency services).
Pre-exposure prophylaxis
Pre-exposure prophylaxis (PrEP) medication is taken before exposure to HIV to prevent infection. A national PrEP programme was introduced in Ireland in 2019 with PrEP available free of charge to those considered to be at risk of HIV through sex. PrEP is available in some public sexual health services and through some GP and private providers.
The HSE Sexual Health and Crisis Pregnancy Programme reported that in 2022, 3,388 individuals had free PrEP prescriptions filled (proxy for those on PrEP), and 1,240 were new PrEP users (first ever PrEP prescription). Baseline HIV testing prior to starting PrEP is crucial, since initiation in the context of undiagnosed HIV infection could lead to development of ART resistance.
References on request











Leave a Reply
You must be logged in to post a comment.