There is no gold standard in the management of whiplash-associated disorder, but early proactive, conservative treatment plays an important part in recovery.
Whiplash and whiplash-associated pain is one of the most common musculoskeletal pain issues following traffic accidents. With over 5,000 car and motorbike users injured annually in Ireland, this directly impacts on the urgent and long-term workload for the primary care physician, physiotherapy services, emergency departments, and pain consultants alike. (CSO: data on road safety, 2019).
PIAB data
In 2018 the Personal Injuries Assessment Board (PIAB), the independent state body, which assesses personal injury claims in Ireland, published data on whiplash-related injury compensation awards resulting from road traffic accidents in Ireland. The statistics show that of the 4,500 cases assessed by the PIAB during a six-month period, 70.8 per cent of all personal injury motor cases were whiplash-related (ie 3,100 cases in six months). Over half – 55 per cent – of whiplash cases received a total award of between €10,000 and €20,000 in total damages, and in 88 per cent of whiplash cases the claimant received a total award of under €30,000. This figure is four times the average payment in the UK. More recent figures in Ireland suggest that this is falling. This may be that many individuals are not satisfied with the process and escalate proceedings.
Clinical features
Whiplash-associated disorder (WAD) is the official name for the constellation of symptoms affecting the neck that are triggered by an accident with an acceleration–deceleration mechanism. WAD is typical in motor vehicle accidents, specifically with an impact from behind or from the flanks, but WAD can also result from other injuries including diving, falls or a blow to the head. The Quebec Task Force on Whiplash-Associated Disorders divides the classification of WAD into five different categories based on pathoanatomical changes in response to trauma. These are listed in Table 1.
| WAD GRADE | FEATURES |
| Grade 0 | • No complaints in the neck. No physical signs |
| Grade I neck pain | • Neck pain • Stiffness/tenderness, no physical signs • Minimal influence on daily activities |
| Grade II neck pain | • Neck symptoms • Musculoskeletal signs • Impact on daily activity |
| Grade III neck pain | • Neck symptoms • Presence of neurological disorders, such as decreased reflexes, muscle weakness, or decreased sensory function |
| Grade IV neck pain | • Indications of serious underlying pathology, such as fracture, myelopathy, or neoplasm |
However, the mere existence of neck pain after a motor vehicle accident can conjure doubts regarding the extent of injury and symptoms. The lack of any objective findings on either plain radiographs or MRI of the cervical spine can leave many questions unanswered in regards to aetiology or sources of pain generation.
Clinical signs of WAD typically include localised spasm and tenderness as well as limitation in the active range of motion, including lateroflexion and extension. Patients with neck pain have tenderness and spasms that are not evident in the asymptomatic individuals. Even so, palpation may reveal localised tenderness, and range of motion may be restricted, but neither of these features yield a definitive diagnosis in the WAD I and II patients. They merely point to some abnormality that warrants further interventions.
For many individuals the symptoms of neck stiffness and headache only appear 24 hours after the incident. Many have difficulty in portraying a clear picture of their symptoms.
The clinical profile of WAD appears to be multifactorial. For example, the incidence of acute WAD appears to be most frequent in male drivers aged between 20-and-24-years, while passengers in the same event are most frequently between 15-and-19-years-of-age. Conversely, female gender, older age, neck pain on palpation, and muscle pain appear to be independently associated with a slower recovery from whiplash, as are pain or numbness radiating from the neck to arms, hands or shoulders, and headache. Similarly, Hartling et al suggested that increased age, number of initial physical symptoms, and early development of upper back pain, upper extremity numbness or weakness, and or disturbances in vision, all can contribute to increased risk for developing persistent WAD.
If the case involves litigation, which could raise suspicion regarding a patient’s intent toward recovery vs secondary gain, practitioners fall into groups supporting either a nonorganic or organic model for the symptoms associated with whiplash syndrome, presenting a little grey area in between the groups.
WAD is the result of a biomechanical injury
In the early literature Cowe (1928) coined the term “rail spine” to describe the features we now recognise as ‘whiplash’ because it was used to describe the traumatic cervical injuries specifically induced during a train accident. Historically, authors described the mechanisms of an acceleration-deceleration injury of the cervical spine and suggested that they result in a “lash-like effect” on the cervical vertebral column
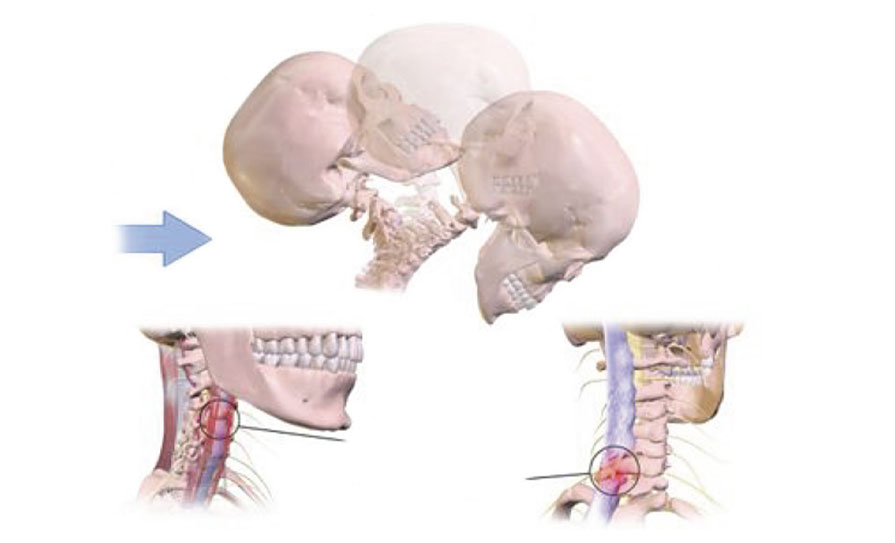
WAD can be explained by considering the biomechanical process experienced during a motor vehicle accident. This type of accident results in injuries to tissues including the intervertebral disc, facet joints, supporting musculature, and ligaments. Clinical features are the tissue response and the patient’s clinical presentation.
For example, in response to a rear-end impact, the occupant’s torso is thrusted forward as it is rapidly contacted by the forward moving seat. This causes a transient S-shaped posturing of the cervical spine, forcing the cervical spine into aphysiologic motions of extension in lower segments and flexion in the upper segments. Energy is stored during this event in the elastic components of the cervical spine, followed by a rapid release of this energy that propels the head and neck forward. This energy release produces subsequent rapid flexion and distraction forces in the cervical spine, lending to further trauma. The consequences of these changes could be profound, as the acceleration forces accompanying aphysiological motion could lead to injury from capsular strain, articular compression, or disc trauma. Moreover, it appears that differences in auto seat stiffness may influence these mechanics and subsequent severity of trauma and symptoms.
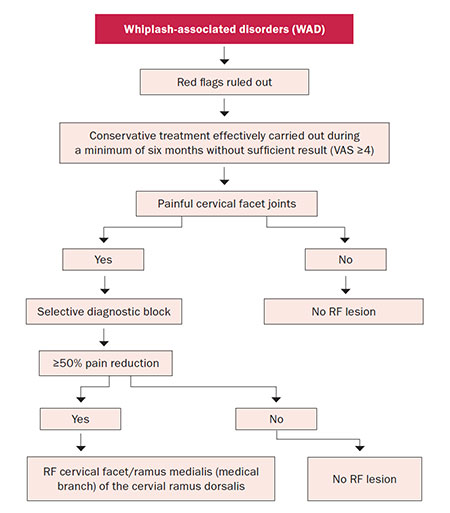
The issue is that the cervical facet joint capsule is well innervated, receiving its nerve supply from the medial branches of the dorsal rami. This nerve supply is comprised of mechanoreceptors and nociceptors, indicating neural input from this spinal structure in proprioception and pain perception. As a consequence of this rich nerve supply, the facet capsule appears to be involved in WAD, as the prevalence of lower cervical facet joint pain in WAD has been reported to be as high as 49 per cent. Notwithstanding, diagnostic blocks and radio frequency lesions have been used to suggest and support the role of the cervical facet joint as one of the most common sources of chronic neck pain after whiplash (Figure 3).
Management of WAD
There is no gold standard in the management of WAD, but early proactive, conservative treatment plays an important part of regaining control of the situation.
a) Investigations
Research has demonstrated that an MRI scan during the chronic stage of a whiplash injury rarely shows a traumatic defect. Choosing an MRI is guided by clinical evaluation in case of unexplained neurologic abnormalities and in preparation of surgical intervention. MRI is perhaps the best screening tool for missed and occult fractures, infections, and tumours. Apart from these criteria, utility of MRI is limited.

b) Proactive conservative treatment
Assuming that there are no mechanical red flags to explain the underlying the pain, then active rehabilitation is encouraged. While caution should be exercised when estimating the efficacy of conservative treatments in patients with whiplash injury, active interventions appear to be more effective vs passive management strategies in patients with whiplash injury.
- Encourage returning to activity.
- Regular and consistent activity is more likely to result in a positive resolution.
- Individuals should be informed that recovery can take up to six weeks to resolve in some cases and that compliance, in so far as possible, to treatment is important.
- Movement restoration can be achieved through a combination of manual therapy and active exercise. Manual therapy utilises passive movement techniques or mobilisation and manipulation to restore joint mobility and reduce pain. For the treatment of acute whiplash syndrome, joint-specific mobilisation treatment combined with exercise provides a significantly better outcome than exercise alone. Early patient participation in an active physiotherapy programme that emphasises active mobilisation has been proven to achieve improved pain reduction and increased cervical mobility compared with control groups prescribed with two weeks rest and a soft cervical collar. The use of therapeutic exercise should focus on restoring normal function of the cervical spine through coordination and activation exercises.
- The use of a cervical collar is not recommended, particularly in the acute stages of whiplash. In fact, early active exercise has proved to be statistically superior to traditional, conservative soft collar use over a six-month period in terms of pain and self-reported disability after whiplash injury. Therefore, there is no evidence that cervical collars provide any long-lasting benefits and their use should be limited to the acute stage of symptoms.
- The whiplash patient often presents with limited range of movement and significant apprehension due to fear-avoidance behaviour. The avoidance of normal neck movement can result in the ‘disuse syndrome’, contributing to muscle atrophy and impaired motor pool firing. The application of active treatments has been related to reduction of neck pain and self-experienced benefits for patients with chronic neck pain.
- Prescription of mild-to-moderate regular analgesics can allow the individual get the best response and improve recover periods is sensible. In general the use of products such as non-steroidal anti-inflammatory medication (NSAIDs) (if not contraindicated) combined with another product such a tramadol or low-dose codeine could provide the short-term control required. This can provide the degree of relief required in the early phase. A risk-benefit analysis should be considered where long-term use of analgesics are required.
c) Interventional options
For many patients suffering from WAD, conservative management is not enough and recovery can be maximised through invasive pain control measures. These interventions should be focused on the most likely cause for the pain.
- Typically, cervical facets injection or radio frequency denervation, cervical epidural, and/or targeted musculoskeletal injections are all key options. These procedures are not without risk but when undertaken under x-ray or ultrasound guidance they can provide enormous improvements within a short time-frame. A correctly-chosen procedure can provide significant improvement in outcome measures such as a pain intensity, neck disability index, and patient satisfaction. Radio frequency denervation can provide three-times longer duration of pain relief compared to injections. Figure 2 outlines a simple WAD management pathway algorithm.
- Local injections to the musculoskeletal tissues can provide the additional relief required. These are best provided under direct vision with ultrasound guidance. The injection of steroid, Botox or platelet-rich plasma can be extremely useful.
- More recently the use of non-invasive bioelectronic devices, such as the BioWave Device has provided excellent practical relief.
- The use of therapeutic exercise should focus on restoring normal function of the cervical spine through coordination and activation exercises.
Conclusion
WAD is a real entity that can impact profoundly on the daily activity of normal living for those affected. WAD can have enormous consequences for the individual and the healthcare provider. However, Spitzer et al indicates that the natural course of whiplash is fairly favourable. Approximately 85 per cent of the patients resumed their activities within six months after an accident. It is generally assumed that the symptoms become chronic in 15-to-30 per cent of WAD patients. Early recognition and proactive rehabilitation can play a key role in reversing WAD quickly and effectively for your patients.
References (** = high value reference)
Aprill C, Bogduk N. The prevalence of cervical zygapophyseal joint pain. A first approximation. Spine. 1992;17:744–748
Bogduk N. The clinical anatomy of the cervical dorsal rami. Spine. 1982;7:319–330
Bronfort G, Evans R, Nelson B, Aker PD, Goldsmith CH, Vernon H. A randomised clinical trial of exercise and spinal manipulation for patients with chronic neck pain. Spine. 2001;26:788–799
Crowe HE. Injuries of the cervical spine. Presented at the Western Orthopaedic Association, San Francisco, California, 1928
Haldeman S, Carroll L, Cassidy JD, et al. The bone and joint decade 2000– 2010 taskforce on neck pain and its associated disorders: Executive summary. Spine. 2008;33:S5– S7
Hartling L, Pickett W, Brison RJ. Derivation of a clinical decision rule for whiplash-associated disorders among individuals involved in rear-end collisions. Accid Anal Prev. 2002;34:531–539
Lord SM, Barnsley L, Wallis BJ, Bogduk N. Chronic cervical zygapophyseal joint pain after whiplash: A placebo-controlled prevalence study. Spine. 1996;21:1737–1744
Lord SM, Barnsley L, Wallis BJ, McDonald GJ, Bogduk N. Percutaneous radio-frequency neurotomy for chronic cervical zygapophyseal-joint pain. N Engl J Med. 1996;335:1721–1726
McKinney LA, Doman JO, Ryan M. The role of physiotherapy in the management of acute neck sprains following road-traffic accidents. Arch Emerg Med. 1989;6:27– 33
Mealy K, Brennan H, Fenelon GC. Early mobilisation of acute whiplash injuries. BMJ. 1986;292:656–657
Olivegren H, Jerkvall N, Hagstrom Y, Carlsson J. The long-term prognosis of whiplash-associated disorders (WAD). Eur Spine J. 1999;8:366–370
Peeters GG, Verhagen AP, de Bie RA, Oostendorp RA. The efficacy of conservative treatment in patients with whiplash injury: A systematic review of clinical trials. Spine. 2001;26:E64–E73
Rosenfeld M, Gunnarsson R, Borenstein P, Cassidy D. Early intervention in whiplash-associated disorders. Spine. 2000;25:1782–1787
Sandmark H, Nisell R. Validity of five common manual neck pain provoking tests. Scand J Rehabil Med. 1995;27:131–136
Schnabel M, Ferrari R, Vassiliou T, Vassiliou T, Kaluza G. Randomised, controlled outcome study of active mobilsation compared with collar therapy for whiplash injury. Emerg Med J. 2004 May;21(3):306-10
Sizer Jr P, Poorbaugh K, Phelps V. Whiplash associated disorders: Pathomechanics, diagnosis, and management. Pain Pract. 2004 Sep;4(3):249-66**
Suissa S, Harder S, Veilleux M. The relation between initial symptoms and signs and the prognosis of whiplash. Eur Spine J. 2001;10:44–49
Taimela S, Takala EP, Asklof T, Seppala K, Parvi- ainen S. Active treatment of chronic neck pain: A prospective randomised intervention. Spine. 2000;25:1021–1027
van Suijlekomh H, Mekhail N, Patel N, Van Zundert J, van Kleef M, Patijn J. 7. Whiplash-associated disorders. Pain Pract. 2010 Mar-Apr;10(2):131–136 (**)
Van Terf M, de Meij N, Kessela A, Patiin J, Weber W et al. Efficacy and long-term effect of radio frequency denervation in patients with clinically diagnosed cervical facet joint pain: A double-blind randomised controlled trial. Spine. 2021 Mar 1;46(5):285-293
Vendrig AA, van Akkerveeken PF, McWhorter KR. Results of a multimodal treatment programme for patients with chronic symptoms after a whiplash injury of the neck. Spine. 2000;25:238–244
Versteegen GJ, Kingma J, Meijler WJ, ten Duis HJ. Neck sprain after motor vehicle accidents in drivers and passengers. Eur Spine J. 2000;9:547–552
Viano DC. Seat properties affecting neck responses in rear crashes: A reason why whiplash has increased. Traffic Inj Prev. 2003;4:214–227
CSO Road Safety Report. 2019. Available at: www.cso.ie/en/releasesandpublications/ep/p-tranom/transportomnibus2019/ roadsafetyandroadlengths/













Leave a Reply
You must be logged in to post a comment.