A new joint guideline from the American Society of Clinical Oncology (ASCO) and the Society for Integrative Oncology (SIO) outlines evidence-based recommendations on integrative medicine approaches to managing pain in patients being treated for cancer.
A new guideline from the American Society of Clinical Oncology (ASCO) and the Society for Integrative Oncology (SIO) has been published to address gaps in healthcare providers’ knowledge of how to safely and effectively treat common cancer symptoms and side-effects using integrative medicine approaches.
Integrative medicine, defined as the coordinated use of evidence-based complementary practices and conventional care treatments, includes interventions such as acupuncture, massage, meditation, and yoga, which are increasingly available in cancer centres and are recommended for symptom and pain management.
“Pain is a clinical challenge for many oncology patients and clinicians, and there’s a growing body of evidence showing that integrative therapies can be useful in pain management. But to date there has not been clear clinical guidance about when and when not to use these approaches,” said Dr Heather Greenlee, ND, PhD, co-chair of the SIO Clinical Practice Guideline Committee.
Pain in cancer
Pain is one of the most common, disabling, and feared symptoms experienced by patients diagnosed with cancer. Among patients with advanced cancer, pain can be a result of tumour burden or invasion of bones, muscles, or nerves. In addition, many conventional cancer treatments such as surgery, chemotherapy, radiotherapy, immunotherapy, or hormonal therapy can result in both acute and chronic pain conditions, such as aromatase inhibitor-induced joint pain or chemotherapy-induced peripheral neuropathy (CIPN) pain. With improved oncologic treatment, many patients diagnosed with advanced cancer now live longer with symptomatic illness and ongoing oncologic treatment. Additionally, increasing numbers of patients experience remission. Many survivors, however, continue to experience chronic pain resulting from their cancer treatment that not only negatively affects their quality-of-life, but also their daily functions. Chronic pain may also lead to non-adherence to oncologic treatment such as hormonal therapies, thus potentially compromising overall survival. Therefore, effective pain management is of critical importance throughout the cancer care trajectory.
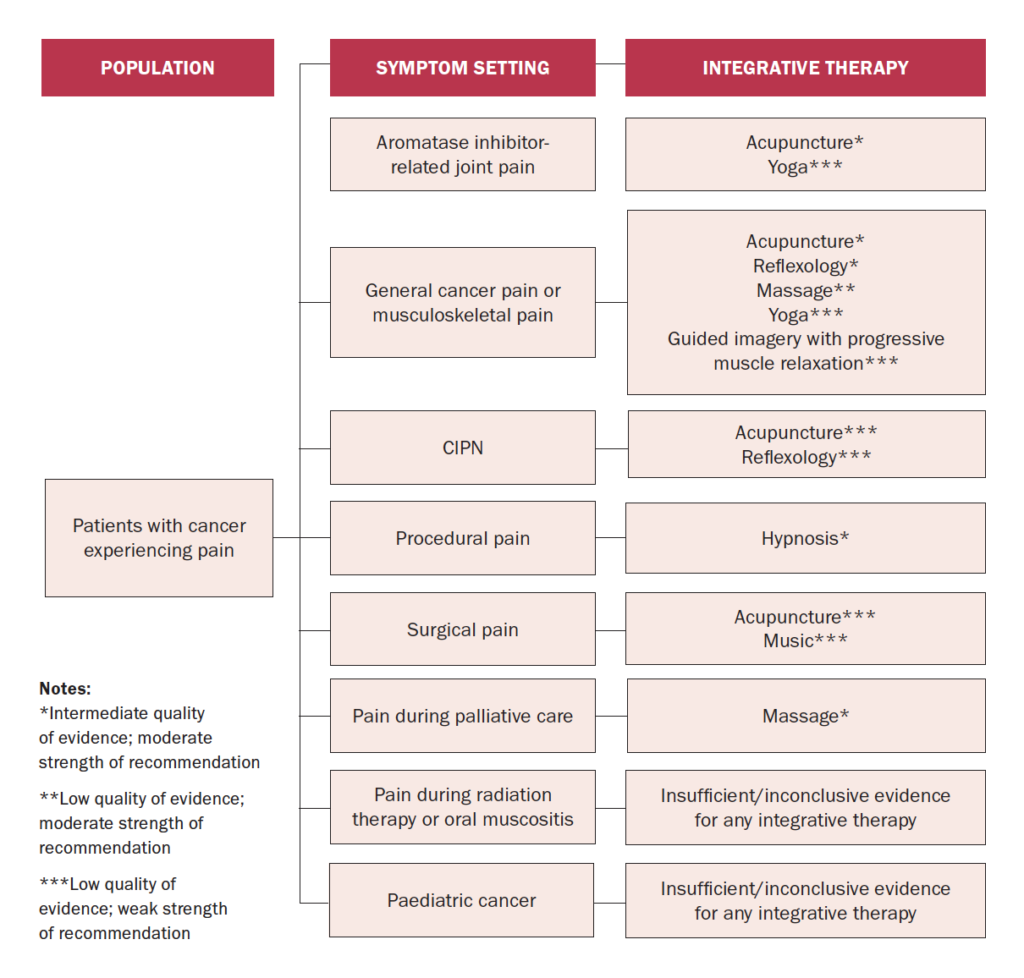
Source: Integrative Medicine for Pain Management in Oncology: SIO–ASCO Guideline
Multidisciplinary approach needed
As pain in patients and survivors of cancer is complex with different aetiologies (eg, tumour burden, treatment-related, and non–cancer-related) and varying presentations (eg, neuropathic and musculoskeletal) and duration (eg, acute and chronic), pain management requires an interdisciplinary approach and should include both pharmacologic and non-pharmacologic treatments, where appropriate, the guideline notes.
An estimated 40 per cent of patients with cancer use integrative medicine on an annual basis (US data). The key guiding principle of integrative medicine is to use these interventions along with conventional pain management approaches (eg, medications, radiation, injections, and physical therapies) and it is not intended to replace conventional interventions, SIO and ASCO point out.
A growing number of randomised controlled trials (RCTs) have found that interventions such as acupuncture or massage can alleviate pain in patients and survivors of cancer. However, for many other interventions, trials are small and are often limited by a lack of methodologic rigor, ASCO and SIO note.
To guide a patient-centred and evidence-based approach to pain management incorporating integrative medicine interventions for appropriate indications, clinicians and patients need to be equipped with knowledge of the current evidence-base of these therapies for pain management in cancer care.
The purpose of this new joint guideline from SIO and ASCO was to systematically appraise the evidence from RCTs, systematic reviews, and meta-analyses, and to provide guidance to clinicians on the effectiveness of integrative medicine treatment options for pain in adults and children with a cancer diagnosis. SIO and ASCO convened an expert panel of integrative oncology, medical oncology, radiation oncology, surgical oncology, palliative oncology, social sciences, mind-body medicine, nursing, and patient advocacy representatives to aid the process. The literature search included systematic reviews, meta-analyses, and RCTs published from 1990 through 2021.
Outcomes of interest included pain intensity, symptom relief, and adverse events. Expert panel members used this evidence and informal consensus to develop evidence-based guideline recommendations. The literature search identified 227 relevant studies to inform the evidence-base for this guideline.
Acupuncture was the most frequently identified intervention at 51 articles, compared with massage in 14 articles. In patients with general cancer pain or musculoskeletal pain, one study with 360 patients randomised them 2:1:1 to either receive electroacupuncture, auricular acupuncture, or usual care. Electroacupuncture reduced pain by 1.9 points on a 0-10 numeric pain rating scale and auricular acupuncture reduced pain by 1.6 points compared with usual care. These results were also durable at six months and associated with minimal toxicities, therefore the panel recommended these interventions for patients with general cancer pain.
Recommendations
In summary, among adult patients, acupuncture should be recommended for aromatase inhibitor–related joint pain, according to the guideline. Acupuncture or reflexology or acupressure may be recommended for general cancer pain or musculoskeletal pain. Hypnosis may be recommended to patients who experience procedural pain. Massage may be recommended to patients experiencing pain during palliative or hospice care.
These recommendations are based on an intermediate level of evidence, benefit outweighing risk, and with moderate strength of recommendation, ASCO and SIO note. The quality of evidence for other mind-body interventions or natural products for pain is either low or inconclusive. There is insufficient or inconclusive evidence to make recommendations for paediatric patients. More research is also needed to better characterise the role of integrative medicine interventions in the care of patients with cancer.
Aromatase inhibitor (AI)–related joint pain
Recommendation 1.1.
Acupuncture should be offered to patients experiencing AI-related joint pain in breast cancer (Type: Evidence-based, benefits outweigh harms; Evidence quality: Intermediate; Strength of recommendation: Moderate).
Recommendation 1.2.
Yoga may be offered to patients experiencing AI-related joint pain in breast cancer (Type: Evidence-based, benefits outweigh harms; Evidence quality: Low; Strength of recommendation: Weak).
General cancer pain or musculoskeletal pain.
Recommendation 1.3.
Acupuncture may be offered to patients experiencing general pain or musculoskeletal pain from cancer (Type: Evidence-based, benefits outweigh harms; Evidence quality: Intermediate; Strength of recommendations: Moderate).
Recommendation 1.4.
Reflexology or acupressure may be offered to patients experiencing pain during systemic therapy for cancer treatment (Type: Evidence-based, benefits outweigh harms; Evidence quality: Intermediate; Strength of recommendation: Moderate).
Recommendation 1.5.
Massage may be offered to patients experiencing chronic pain following breast cancer treatment (Type: Evidence-based, benefits outweigh harms; Evidence quality: Low; Strength of recommendation: Moderate).
Recommendation 1.6.
Hatha yoga may be offered to patients experiencing pain after treatment for breast or head and neck cancers (Type: Evidence-based, benefits outweigh harms; Evidence quality: Low; Strength of recommendation: Weak).
Recommendation 1.7.
Guided imagery with progressive muscle relaxation may be offered to patients experiencing general pain from cancer treatment (Type: Evidence-based, benefits and harms not assessable; Evidence quality: Low; Strength of recommendation: Weak).
Chemotherapy-induced peripheral neuropathy
Recommendation 1.8.
Acupuncture may be offered to patients experiencing chemotherapy-induced peripheral neuropathy from cancer treatment (Type: Evidence-based informal consensus, benefits outweigh harms; Evidence quality: Low; Strength of recommendation: Weak).
Recommendation 1.9.
Reflexology or acupressure may be offered to patients experiencing chemotherapy-induced peripheral neuropathy from cancer treatment (Type: Evidence-based, benefits outweigh harms; Evidence quality: Low; Strength of recommendation: Weak).
Procedural or surgical pain
Recommendation 1.10.
Hypnosis may be offered to patients experiencing procedural pain in cancer treatment or diagnostic workups (Type: Evidence-based, benefits outweigh harms; Evidence quality: Intermediate; Strength of recommendation: Moderate).
Recommendation 1.11.
Acupuncture or acupressure may be offered to patients undergoing cancer surgery or other cancer-related procedures such as bone marrow biopsy (Type: Evidence-based informal consensus, benefits outweigh harms; Evidence quality: Low; Strength of recommendation: Weak).
Recommendation 1.12.
Music therapy may be offered to patients experiencing surgical pain from cancer surgery (Type: Evidence-based, benefits outweigh harms; Evidence quality: Low; Strength of recommendation: Weak).
Pain during palliative care
Recommendation 1.13.
Massage may be offered to patients experiencing pain during palliative and hospice care (Type: Evidence-based; benefits outweigh harms; Evidence quality: Intermediate; Strength of recommendation: Moderate).
Reference
Mao JJ, Ismaila N, Bao T, Barton D, Ben-Arye E, Garland EL, et al. Integrative medicine for pain management in oncology: Society for Integrative Oncology-ASCO Guideline. J Clin Oncol. 2022 Sep 19:JCO2201357. doi: 10.1200/JCO.22.01357











Leave a Reply
You must be logged in to post a comment.