Early detection of malignant melanoma remains a crucial factor in reducing mortality
Skin cancer is the most common cancer in Ireland, with 11,660 cases diagnosed in 2019. Melanoma is a serious form of skin cancer that develops from pigment-producing cells found in the upper layer of skin known as melanocytes. Less common than basal cell (BCC) and squamous cell carcinomas (SCC), melanoma is more serious because of its ability to spread rapidly to other organs, if not treated at an early stage. Melanoma is usually curable when it is detected and treated early. Once a melanoma has spread deeper into the skin or other parts of the body, it becomes more difficult to treat and can be fatal.
Excluding non-melanoma skin cancers, melanoma is the fourth most common cancer in Ireland, with approximately 160 deaths and 1,100 new cases diagnosed each year. From once being a rare cancer, the average lifetime risk for melanoma has now reached one-in-50 in many Western populations. Since the 1960s the incidence of melanoma has increased in Caucasian populations and become one of the most frequent cancers in fair-skinned populations. Australia and New Zealand have the highest incidence of melanoma in the world and there are also high rates in Northern Europe and North America. It is less common in Asia, Africa, and Latin America.
Statistics from the National Cancer Registry Ireland (NCRI) show that the incidence of melanoma in Ireland continues to rise. With approximately 20 cases diagnosed per 100,000 persons per year, rates have increased by over 5 per cent per year in men since 1994, while female incidence rates have also increased over time, but at a lower rate of 2.7 per cent per year. Since 1994, mortality rates for melanoma in Ireland have increased by 2.3 per cent annually in females and 4.7 per cent per year in males.


Unlike other solid tumours, melanoma mostly affects young and middle-aged people. The median age of diagnosis is 57 years and the incidence increases linearly after the age of 25 years until the age of 50 years and then slows, especially in females. More than a quarter of melanoma skin cancers are diagnosed in people under the age of 50.
Melanomas typically occur on the skin but may also rarely occur in the mouth, intestines, eye (uveal melanoma), underneath a nail or on the sole of the foot. They occur most commonly on the legs in women and on the back in men.
Melanoma is considered a multi-factorial disease arising from an interaction between genetic susceptibility and environmental exposure.
The primary cause of melanoma is ultraviolet light (UV) exposure in those with low levels of the skin pigment melanin. When skin is exposed to UV radiation from the sun or tanning beds, it causes skin damage, which triggers melanocytes to produce more melanin. Eumelanin and pheomelanin are two types of melanin in the skin. While eumelanin has the ability to protect the skin from sun damage, pheomelanin does not. Fair-skin contains more pheomelanin and darker-skin contains more eumelanin. People with fair skin are more susceptible to sun damage, burning and developing melanoma than dark-skinned people due to a lack of eumelanin. Melanoma occurs when DNA damage caused by UV radiation triggers mutations in the melanocytes, resulting in uncontrolled cellular growth.
Other factors contributing to an increased risk of developing a melanoma include being immunosuppressed, a family history of melanoma, a previous diagnosis of skin cancer, previous skin damage caused by sunburn or radiotherapy treatment, and phenotypic characteristics such as pale skin, red or blonde hair, blue eyes and a large number of freckles. Repeated sunburn, either by the sun or artificial sources of light, increases the risk of melanoma in people of all ages. The risk of developing skin cancer increases with age. Rare genetic conditions such as xeroderma pigmentosum also increase the risk.
The most important host risk factors are the number of melanocytic nevi, family history and genetic susceptibility. Melanocytic nevi commonly known as moles, are benign accumulations of melanocytes or nevus cells and may be congenital or acquired. Approximately 25 per cent of melanoma cases occur in conjunction with a pre-existing nevus. The total nevus count is positively correlated with melanoma risk and varies depending on the number, size, and type of nevi.
There are four main types of skin melanoma; superficial spreading melanoma, nodular melanoma, lentigo maligna melanoma, and acral lentiginous melanoma. Another type called amelanotic melanomas are quite rare.
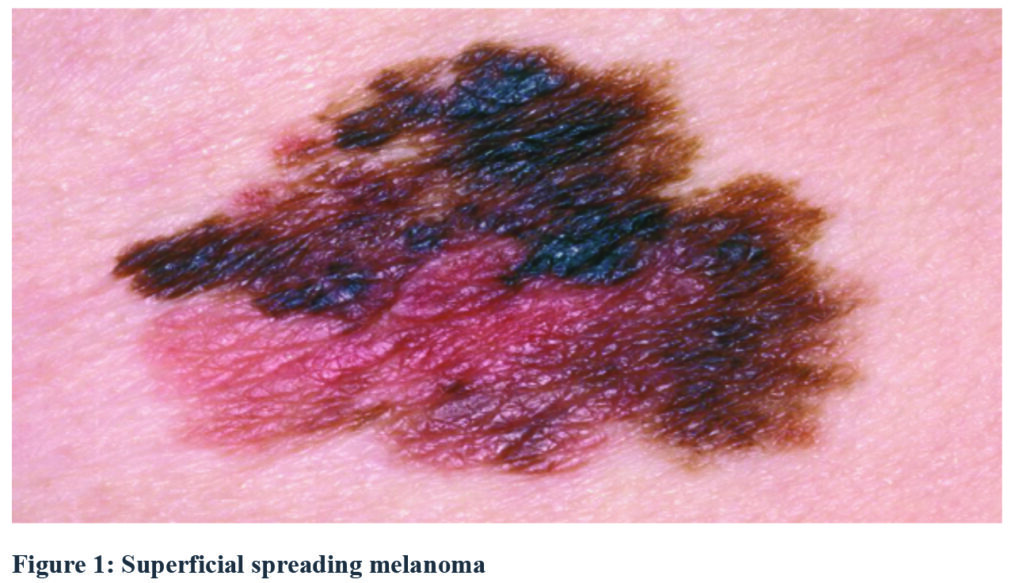
Superficial spreading melanoma
Approximately 70 per cent of all melanomas are superficial spreading melanomas, which are more common in people with pale skin and freckles. They initially tend to grow outwards rather than downwards, however, if they do grow downwards into the deeper skin layers, they can spread to other parts of the body.
Nodular melanoma
Nodular melanomas are faster-developing and can quickly grow downwards into the deeper layers of skin if not removed. They usually appear as a changing skin lump and are often black or red in colour. Nodular melanomas most commonly occur on the head, neck, chest or back, and bleeding or oozing is a common symptom.
Lentigo maligna melanoma
Lentigo maligna melanomas account for approximately 10 per cent of melanomas. They most commonly affect older people, especially those who have spent a lot of time outdoors. They develop slowly over a number of years and appear on areas that are often exposed to the sun, such as the face. Lentigo maligna melanomas are initially flat and develop sideways on the surface layers of skin. They can resemble freckles, but are usually larger, darker and more defined than a normal freckle. They gradually get bigger and may change shape. At a later stage, they can grow downwards into the deeper layers of skin and form nodules.
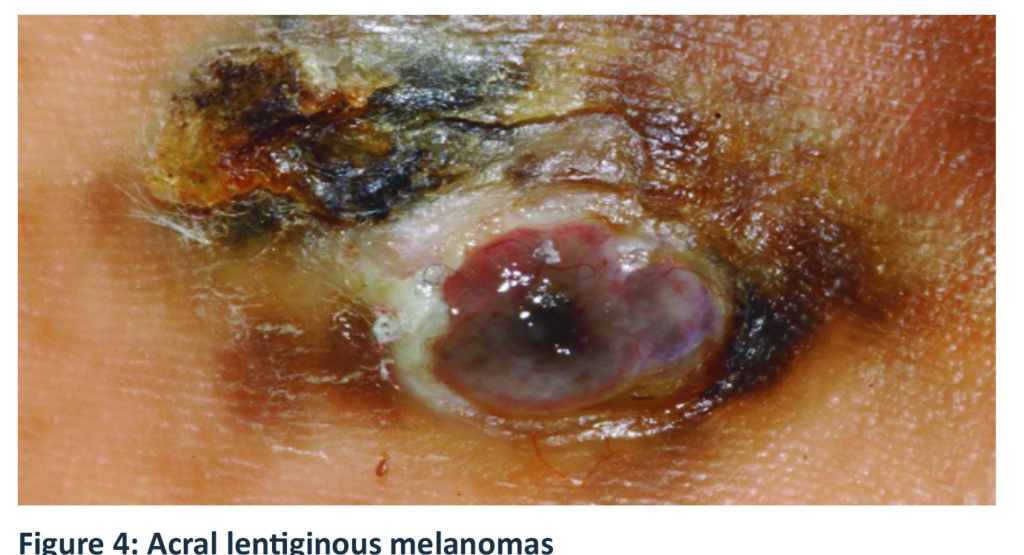
Acral lentiginous melanoma
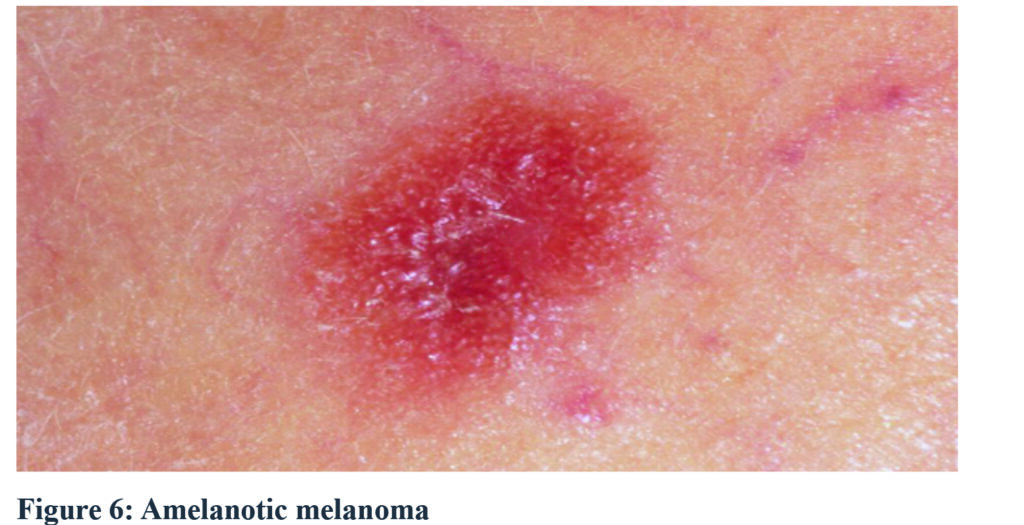
Acral lentiginous melanomas are a rare type of melanoma. They usually occur on the palms of the hands and soles of the feet, but can also develop around a nail, most commonly the thumb or big toenail. They can occur in all skin types, but are most common in people with dark skin. Amelanotic melanomas are also rare, accounting for about five-in-100 melanomas. They usually have little or no colour, but may occasionally be pink or red, or have light brown or grey edges.
Diagnosis and staging
Early detection of malignant melanoma remains a crucial factor in reducing mortality. Compared to other cancers, malignant melanoma has the advantage of its cutaneous location, allowing early detection through non-invasive approaches. Pathological examination however, remains the gold standard for diagnosis. The prognosis is directly proportionate to the depth of the neoplasm, which in turn increases with time.
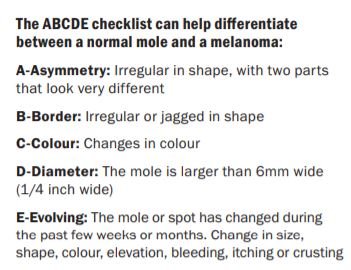
Normal moles (nevi) are usually round or oval, with a smooth edge, and ≤6mm in diameter. The first sign of a melanoma is often a new mole or a change in the appearance of an existing mole. Indications include changes in a mole’s colour, increase in size, irregular edges, itchiness, skin breakdown, and bleeding. Other tools to help improve early diagnosis include the Glasgow seven-point checklist, which includes three major criteria – change in size, shape, colour, and four minor criteria – sensory change, diameter of 7mm or greater, presence of inflammation and crusting or bleeding. This checklist has been less widely adopted than the ABCDE criteria. Another paradigm is the ‘ugly duckling’ sign, based on the perception that a pigmented lesion ‘looks different from all of its neighbours’. This criteria has been shown to be sensitive for melanoma detection.
Referral to a specialist is required if a melanoma is suspected. The melanocytic nevi (mole) will be removed and sent for biopsy (excision biopsy). If cancer is confirmed, another procedure will be required to remove a wider area of skin to make sure the cancerous cells have been removed. Further tests will be carried out if there is a concern the cancer has spread into other organs, bones or the bloodstream. Sentinel lymph node biopsy is used to determine whether the cancer has spread beyond the primary into the lymphatic system.
The sentinel nodes are the first lymph nodes into which a tumour drains. Sentinel node biopsy involves injecting a tracer material to locate the sentinel nodes, which are removed and analysed in a laboratory. Because only a few lymph nodes are removed, the risk of lymphoedema is small. If the sentinel nodes are clear of melanoma, the cancer is unlikely to have spread, and removing additional lymph nodes is unnecessary.
If cancer is detected surgery to remove the remaining lymph nodes (completion lymph node dissection or completion lymphadenectomy) is performed. Other tests carried out include CT scan, MRI scan, PET scan, and blood tests.
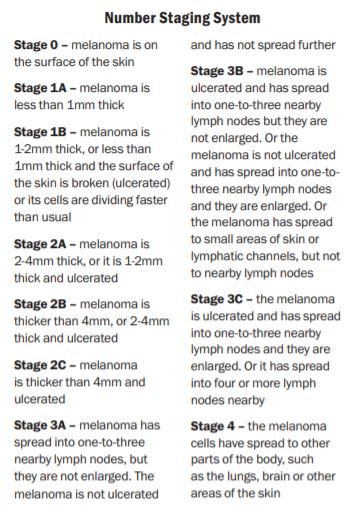
Staging of a melanoma determines how deep it has grown and how far it has spread. Different systems used include the TNM (tumour, node, metastasis), number staging system (0-4) or the Clark or Breslow scale to describe how deeply the melanoma has gone into the skin.
Treatment
Treatment of melanoma can include single or combined therapies, depending on the patient’s health, stage, and location of the tumour. Therapeutic approaches include surgical resection, chemotherapy, photodynamic therapy, immunotherapy, biochemotherapy, and targeted therapy. The main treatment for melanoma is surgery, and if diagnosed and treated at an early stage, surgery is usually successful. Radiotherapy after surgery usually consists of a course of five treatments a week for a number of weeks. Chemotherapy is now rarely used to treat melanoma and targeted treatments and immunotherapy are the preferred treatment options.
If undiagnosed until an advanced stage (stage IV), treatment is given to help slow the cancer’s growth, reduce symptoms, and extend life expectancy. This usually involves treatment that targets specific genetic changes in the melanoma, such as BRAF inhibitors, or checkpoint therapies that boost the body’s immune responses to the melanoma.
If a melanoma has spread to other parts of the body, the prognosis is less favourable. Metastatic melanoma isone of the most serious types of skin cancer, and accounts for most skin cancer deaths in Ireland. The five-year survival rate for patients with stage IV melanoma is under 20 per cent, compared with over 50 per cent if the disease is diagnosed at stage III. Unresectable cancers cannot be removed through surgery.
Newer treatments such as immunotherapy and targeted treatments are showing encouraging results in advanced melanoma. A number of different medications are available, some of which can be used as a monotherapy or as combination therapy. Immunotherapy medications for advanced melanoma include ipilimumab, nivolumab and pembrolizumab. Approximately 40-to-50 per cent of people with melanoma have gene mutations. Targeted treatments such as vemurafenib, dabrafenib and trametinib can be used to specifically target these gene mutations to help slow or stop the cancer cells growing.
In 2019 the HSE approved reimbursement for encorafenib in combination with binimetinib for the treatment of adults with unresectable or metastatic melanoma with a mutation known as BRAF V600. Just over 1,000 patients in Ireland have melanoma, of whom about half have the BRAF mutation. More than 97 per cent of BRAF mutations are in the BRAF V600 gene. In February this year (2021), after a long advocacy campaign by cancer patients, the HSE also announced that it was to reimburse adjuvant immunotherapies for stage III melanoma patients in Ireland.
While the HSE had been reimbursing three different kinds of immunotherapy drugs for melanoma patients previously, it was only for those who were at a more advanced stage. Instead, stage III patients were continually monitored through a ‘watch and wait’ strategy, though patients with certain private health insurance plans could access these drugs. However, the HSE will now (since 1 February) reimburse nivolumab, which is used as monotherapy for the adjuvant treatment of adults with melanoma, whose cancer involves lymph nodes or metastatic disease, who have undergone complete resection.
Pembrolizumab is also in the process of being approved for reimbursement in this cohort. This can be used as monotherapy for the adjuvant treatment of adults with stage III melanoma and lymph node involvement, who have undergone complete resection also.
Survival and prevention
Survival from melanoma has increased in Ireland since the 1990s due largely to improvements in treatment for late stage tumours, as well as more patients presenting with earlier stage disease. The National Cancer Strategy 2017-2026 outlines the HSE’s plans for cancer prevention and control and prioritises the development of a national skin cancer prevention plan targeting children, outdoor workers, sunbed users and those who pursue outdoor leisure activities. Addressing the rising incidence of skin cancer, the strategy prioritised the need to develop and implement the national skin cancer prevention plan (2019-2022).
Melanoma is not always preventable, but a number of measures can be taken to reduce its occurrence. It is important that people are made aware of the dangers of UV radiation from the sun and artificial sources such as sunbeds. Wearing sunscreen is important and recommended even in winter, using a broad-spectrum, high UVA protection water resistant (UVA/UVB) sunscreen with a sun protection factor (SPF) of at least 30+ for adults and 50+ for children. It is advisable to seek shade and cover the skin as much as possible when in the sun, protect the face, ears and neck with a wide brimmed hat and wear sunglasses. Babies and young children are particularly vulnerable to sun exposure, and should always be kept out of direct sunlight.
Educating people to regularly check their skin and seek help for notable changes, can help lead to an early diagnosis of melanoma and increase the chances of successful treatment. Timely recognition, detection, rapid treatment and follow-up is key to improved outcomes and survival rates from malignant melanoma.
References on request













Leave a Reply
You must be logged in to post a comment.