Sublingual immunotherapy and other updates on adolescent and adult asthma
The prevalence of asthma has been increasing internationally for several decades. Ireland has one of the highest prevalence figures for asthma in the world with estimates approaching half a million people affected. This is disappointing during a time when Ireland has made significant, slow but steady progress, combating tobacco dependence. The reasons behind this shift and the consequent significant burden of illness is not fully understood, but is felt to represent changing environmental factors such as increasing exposure to allergens and reducing bacterial infections in a genetically susceptible population.
Burden of disease
Asthma consistently figures in the most common reasons for hospital admission. Over 90 per cent of these admissions are emergency or unscheduled. Four times as many admissions are treated and presumably discharged home from emergency departments. National intelligence data is for public hospitals only and does not factor in patients attending insurance-funded acute care units or the increasing activity in emergency rooms attached to private hospitals.
At least 20 per cent of patients report poor control of their asthma with impacts on quality-of-life and mortality risk. The Asthma Society of Ireland reports that children lose five school days while adults lose seven work days annually as a result of their asthma. The Irish Thoracic Society reports that mortality rates from asthma increased in the last decade with a five-year standardised mortality rate of 1.92 and notes that these figures are a source of concern.
Definition of asthma
Asthma is defined as an inflammatory disease of the airway. Triggers such as viruses, allergens or exercise, narrow the airway through luminal obstruction, muscle contraction, and structural changes. Patients experience airflow limitation with symptoms of cough, breathlessness, and wheeze.
General principles of treatment
Beta-adrenergic bronchodilators, both short- and long-acting, relax airway smooth muscle tone, increasing luminal diameter and reducing airway obstruction. Glucocorticoids, ideally inhaled, reduce the airway inflammatory response to the asthma trigger, preventing the downstream cascade series of events responsible for daily symptoms and acute exacerbations. Long-acting anti-muscarinic (LAMA) bronchodilators are also licensed for the treatment of asthma as adjunctive therapy in more severe cases. Immunisation helps mitigate airway infections while identification of individual triggers such as exercise or inhalation of cold air can help manage specific triggers for a given patient. The importance of allergen management has been recognised for many years, but is often limited to avoidance strategies that are hampered by the ubiquity of sensitising allergens such as house dust mite or airborne pollens.
The role of immunotherapy
Desensitisation to specific allergens has been feasible and practised back to the early part of the last century. This approach works by reducing the inflammatory response to a sensitised antigen and represents an intervention early in the pathway from triggering agent exposure through to symptomatic disease. The appeal of this approach was tempered by the need to administer desensitising doses of antigen parenterally with anaphylaxis, collapse, and death rare, but much feared adverse events in published reports. As a result immunotherapy was restricted to specialised centres or clinics with logistic and medical infrastructure designed to manage such risks safely. An alternative administration route, specifically sublingually delivering desensitising doses of antigen topically under the tongue was developed. Sublingual immunotherapy (SLIT) delivers comparable reductions in allergen reactivity with a more acceptable side-effect profile. Widespread implementation of this approach has been hampered by the need to prepare allergen solutions by specialist manufacturers, which are dispensed in bottles with a prescribed number of drops of allergen solution administered each day. Allergen tablets with consistent and biologically standardised doses of allergen have been developed, which extend the scope of immunotherapy from specialist clinics to general respiratory and ENT services and into primary care for GPs with an interest in allergic airway disease. In Ireland this therapeutic approach was limited to SLIT for grass pollen allergy, however, house dust mite and tree pollen products are scheduled to be available imminently.
The Global Initiative for Asthma
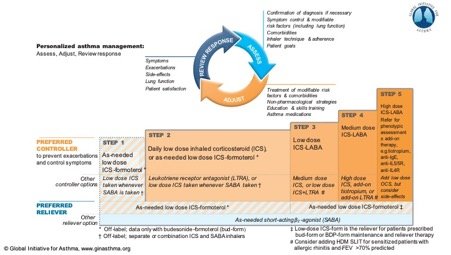
The Global Initiative for Asthma (GINA) is an international self-funded collaboration of major pulmonary and health organisations dedicated to improving knowledge and treatment of asthma worldwide. GINA produces a regularly updated set of evidence-based management principles with the most recent iteration produced in 2019.
Traditionally asthma management has been seen as an escalating stepwise series of interventions beginning with short-acting bronchodilators with subsequent increments of inhaled steroids and long-acting bronchodilators. Adjunctive and systemic therapy is reserved for those with more severe disease and most likely attending secondary or tertiary care clinics.
A major change at Step One
The most radical development of the new GINA document is the abandonment of short-acting bronchodilators alone as acceptable therapy for the management of asthma. A review of published studies identified that treatment with short-acting bronchodilators alone was associated with a risk of sudden exacerbation and death that was mitigated by the use of any inhaled steroid. As a result Step One of the GINA report now states that patients with symptoms twice per month or less should use a combined inhaled corticosteroid and long-acting beta adrenergic bronchodilator (ICS/LABA) as required. Budesonide/formoterol is the recommended combination as most of the relevant studies have focused on this pairing, however, the authors note that beclomethasone/formoterol may also be appropriate.
Step Two
For patients with more frequent or persistent symptoms regular low-dose ICS are recommended. This can pose some challenges as it de-emphasises the role of the combined inhaler, which may be reintroduced if the patient has to proceed to higher treatment steps for adequate symptom control. The use of ICS/LABA is considered off-licence at this step although studies have shown non-inferiority when compared with ICS alone. In practice the patient may oscillate between Step One and Step Two themselves in the absence of medical supervision. Irrespective, the use of more regular ICS at Step Two seems key to success as other agents such as leukotriene receptor antagonists, while useful, appear less efficacious than regular ICS alone for reducing exacerbation frequency. Finally, economic considerations might favour ICS over dual agents at this step as exacerbation rates are similar though the time taken to establish control is shorter when the dual agent is used.
Step Three
Step Three is unchanged in the 2019 document with a definite role for regular ICS/LABA. For patients with more than one exacerbation in the previous year, maintenance and reliever treatment with inhaled budesonide/formoterol or beclomethasone/formoterol produces superior results to short-acting bronchodilator and regular ICS with or without a long-acting bronchodilator. Mixing inhaled ICS/LABA formulations (ie, one ICS/LABA for maintenance and a different ICS/LABA for relieving) is not recommended and patients using a maintenance LABA other than formoterol should be prescribed a short-acting bronchodilator for intermittent use. At this step SLIT may be considered for patients on appropriate symptomatic therapy with rhinitis who are allergic to house dust mite, provided FEV1 is >70 per cent.
Step Four
Further escalations at Step Four include the addition of tiotropium via mist inhaler, leukotriene antagonists, and increasing the dose of ICS. SLIT is also considered at this step if it has not been utilised at an earlier stage.
Step Five
Patients at Step Five generally require management in a specialist clinic with access to biologic therapy including anti-IgE (omalizumab), anti-IL5 (mepolizumab), anti-IL5R (benralizumab), anti-IL4R (dupilumab), and oral corticosteroids.
Other management considerations
The fundamentals of good asthma management apply across the spectrum of disease from mild to severe, but particularly beyond Step Two. These include avoidance of triggers including smoking, inhaler technique, compliance with treatment, and management of comorbidities such as gastro-oesophageal reflux disease (GORD). Failure to respond to an appropriate intervention should prompt a review of diagnostic assumptions and consideration of other entities such as asthma/COPD overlap syndrome.
The one airway hypothesis
Pathology of the upper airway should also be considered as part of the management of asthma. Upper airway disease can be considered a comorbid condition complicating asthma, however, the overlap of triggers and treatment responses suggests a more intimate association. The one airway hypothesis was proposed widely in the 1990s and suggested the respiratory epithelium was a single and continuous structure from the nose right through to the respiratory bronchioles. Pathophysiological processes are equally pertinent and prevalent in the upper and lower airways and indeed causally interdependent. While this seems an oversimplification of the asthmatic airway it does provide a useful paradigm for the management of more complex asthma patients and is certainly reflected in the observation of allergic rhinosinusitis preceding an unstable period of asthmatic airway tone. Upper airway disease is reported by up to three-quarters of patients with asthma, particularly those with atopic or allergic disease. Simple nasal washes have been shown to reduce asthma symptom scores as well as improving upper airway symptoms in suitably selected patients. Topical steroids, antihistamines, and leukotriene receptor antagonists can all improve asthma control in part by reducing the upper airway inflammatory response. SLIT has a role in both upper and lower airway disease once suitable allergens are identified.
The clinical history and antigen exposure
A clear and focused history will often suggest if allergy or atopy is contributing to asthma symptoms and may also increase the confidence of the asthma diagnosis. Sensitisation generally requires repeated exposure and a careful enquiry into occupational and domestic exposures can identify suspected antigens. Geography also plays a role. For example, olive tree pollen poses a significant challenge for Mediterranean populations, but is seen only under exceptional circumstances in an Irish context. Seasonality and timing of exposure is also important. Symptoms worsening in summer months are easily identified as manifestations of grass pollen allergy (typically Timothy and Rye varieties). Tree pollen allergy is less often considered and can cause an otherwise inexplicable deterioration in control as early as February. Hazel, Alder, and Birch are particular considerations though any flowering tree may be responsible and a modicum of arboreal familiarity can prove invaluable. House dust mite is a perennial allergen, which can cause year-round symptoms in heavily exposed susceptible individuals. A surge in symptoms is, however, seen around autumn when indoor temperatures and humidity increases, favouring the proliferation of mites and subsequent antigenic load.
Appropriate allergy testing
When an allergic trigger is suspected, confirmatory testing is required as allergen avoidance can be both costly and time-consuming. Testing should be guided by history and clinical suspicion as blanket or otherwise uninformed testing may produce spurious results leading to ineffective management strategies. As a rule food-based or ingested allergens are only rarely significant in adults with the vast majority of triggers being inhaled or aero-allergens. Serologic testing can be performed by measuring IgE specific antibodies. Total IgE levels may be normal and should not preclude more detailed analysis if the clinical suspicion remains high. Skin prick testing is available in many laboratories and correlates closely, but not exactly with serologic testing. Candidate allergens for testing must be chosen on the basis of history and clinical suspicion. The choice of serology or skin prick test will largely be determined by availability and local resources. Skin prick testing offers the advantage of immediate results at a lower cost and can easily be performed by suitably trained individuals as part of a clinical review. Blood IgG measurement has no place in the management of atopic asthma although precipitating antibodies have a role in the diagnosis of allergic bronchopulmonary aspergillosis in specialist clinics.
SLIT in clinical practice
SLIT for house dust mite in mild-to-moderate asthma was associated in one large study with a small, but significant reduction in inhaled steroid dose at one year without a deterioration in asthma control as evidenced by lung function, quality-of-life scores, and exacerbation rate.
A second study examined patients with poorly controlled asthma despite ICS use and found a reduction in the risk of moderate to severe exacerbation. There were no reports of severe allergic reaction to treatment although mild-to-moderate oral pruritus was frequently encountered. In practice the first dose of immunotherapy is administered in a healthcare setting although subsequent uninterrupted daily treatments appear to be safely administered at home.
Conclusion
Asthma remains a highly prevalent and burdensome condition both for patients and healthcare systems. The pattern of disease is highly variable ranging from sporadic or purely seasonal symptoms through to highly complex presentations. Care is required as patients can transition from mild unobtrusive symptoms to life-threatening exacerbations relatively rapidly. Treatment and advice continues to evolve with new treatment options becoming available across all levels of care from general practice through to subspecialty clinics.













Leave a Reply
You must be logged in to post a comment.