Acne is one of the most prevalent skin conditions globally, affecting a significant portion of the population. It is more common in adolescents, with studies indicating that approximately 85 per cent of individuals between the ages of 12 and 24 years experience some form of acne.
However, it can persist into adulthood, affecting both men and women. While acne is most prevalent during puberty due to hormonal changes, it can also occur in adults. Women are more likely to experience adult-onset acne, often related to hormonal fluctuations, such as those during menstruation or pregnancy.
Psychosocial impact: Acne can have significant psychosocial effects, leading to issues such as low self-esteem, anxiety, and depression, particularly in adolescents.
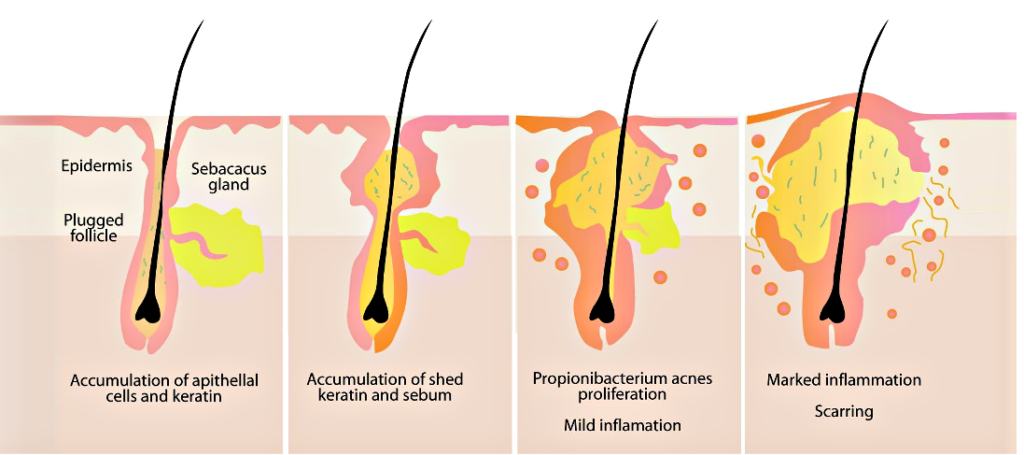
Pathogenesis
The pathogenesis of acne involves several factors, including hormonal changes, skin cell turnover, bacteria, and inflammation.
1. Overproduction of sebum: Hormonal changes, particularly during puberty, lead to increased production of androgens (male hormones), which stimulate the sebaceous (oil) glands in the skin to produce more sebum (oil).
2. Follicular occlusion: The skin cells within hair follicles accumulate in a process known as hyperkeratinisation. This process contributes to the clogging of hair follicles, forming comedones (blackheads and whiteheads).
3. Bacterial growth: The clogged follicles create an anaerobic environment that promotes the growth of Propionibacterium acnes (P acnes), a bacteria normally found on the skin. The proliferation of this bacteria can contribute to inflammation.
4. Inflammation: The immune response to the presence of P acnes and the accumulation of sebum can lead to inflammation. This results in the formation of inflammatory lesions, such as papules, pustules, and cysts.
5. Scarring: In cases of severe acne, the inflammatory process can damage the skin tissue, leading to scarring. This can occur when the lesions rupture or if there is significant inflammation.
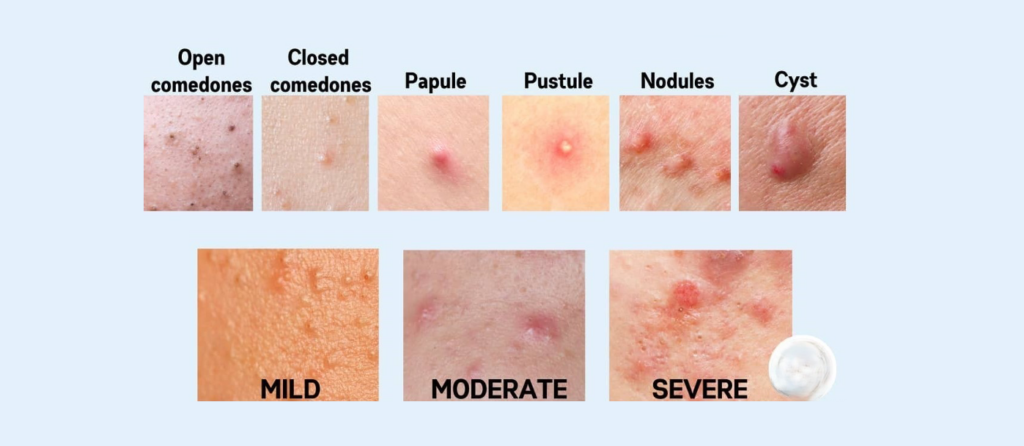
The different stages of pathogenesis give rise to the different individual lesions in acne:
1. Comedones: These are non-inflammatory acne lesions, which include blackheads (open comedones) and whiteheads (closed comedones).
2. Papules: Small, red, raised bumps that can be tender.
3. Pustules: Similar to papules, but filled with pus, often appearing as red spots with a white or yellow centre.
4. Nodules: Large, painful lumps beneath the skin that can last for weeks or months.
5. Cysts: Deep, painful, pus-filled lumps that can cause scarring.
And the individual lesions give rise to the different types of acne, as shown in Figures 3A-D.
Treatment of acne
Acne treatment varies based on the severity and type of acne.




The basics:
▶ Gentle cleansing: Use a mild cleanser to avoid irritating the skin.
▶ Non-comedogenic products: Use makeup and skincare products labelled as non-comedogenic to avoid clogging pores.
▶ Do not pick or squeeze spots: This will increase the risk of scarring.
▶ Diet: There is no evidence to suggest that modifying diet has any effect on acne.
Mild acne (mainly comedones)
Topical treatments:
▶ Benzoyl peroxide: Helps kill bacteria and reduce inflammation, available over-the-counter (OTC).
▶ Salicylic acid: Aids in exfoliating the skin and unclogging pores, available OTC.
▶ Retinoids (tretinoin/adapalene): Promote cell turnover and prevent clogged pores (require a prescription).
▶ Combination (benzoyl peroxide/adapalene).
▶ Topical antibiotics (erythromycin and clindamycin).
Moderate acne (mainly pustules)
▶ Topical antibiotics (erythromycin and clindamycin).
▶ In combination (clindamycin and benzoyl peroxide).
▶ Oral antibiotics: Patients failing to respond to topical antibiotics or combinations require treatment with an oral antibiotic. The ICGP guideline on treatment of acne outlines the following tetracyclines for three months:
• Doxycycline 100mg od.
• Lymecycline 300mg od.
• Minocycline 100mg od.
▶ Trimethoprim at doses of 200–300mgbd is a second-line option for patients failing a tetracycline.
▶ Oral antibiotics should be combined with retinoid/keratolytic agent, this improves activity and helps prevent resistance.
▶ Oral antibiotics should not be used in combination with topical antibiotics as this promotes antimicrobial resistance.
▶ Continue same agent if response and liver function tests should be measured if continued treatment >six months.
Oral contraceptive/anti-androgen
For women who report flaring of acne around their menstrual cycle, the oral contraceptive pill (Dianette) can be very effective.
Spironolactone, which has anti-androgen properties, is also very useful at doses of 50-100mg a day, but female patients must be on effective contraception to avoid feminisation of male foetus.
Severe acne (nodules and cysts)
Patients with severe nodulo-cystic acne require isotretinoin.
Isotretinoin is indicated to treat severe acne, particularly nodular or cystic acne that has not responded to other treatments. Here are some key points regarding isotretinoin:
1. Mechanism of action: Isotretinoin works by reducing the size and activity of sebaceous glands, decreasing sebum production, and promoting the turnover of skin cells. This helps to prevent clogged pores and reduces the growth of P acnes, the bacteria associated with acne.
2. Efficacy: Many patients experience significant improvement in their acne, and for 20 per cent of patients, a single course of isotretinoin can lead to long-term remission. However, results can vary, and some individuals may require additional courses.
3. Side-effects: Isotretinoin can have notable side-effects, falling into two types.
Mild side-effects which are really common:
▶ Dry skin and lips;
▶ Nosebleeds;
▶ Dry eyes;
▶ Increased sensitivity to the sun;
▶ Muscle aches and joint pain;
▶ Potential changes in mood or mental health.
Severe side-effects which are very rare:
▶ Teratogenicity: Due to the risk of severe birth defects, isotretinoin is contraindicated during pregnancy. Women of childbearing age must follow strict guidelines, including using effective contraception before, during, and after treatment.
▶ Hepatitis or pancreatitis (secondary to raised triglycerides): Patients on isotretinoin typically require baseline liver function tests and after commencing treatment.
▶ Potential changes in mood or mental health: A history of any mood disorders should be taken at baseline and any changes during treatment noted. It is important to remember that acne itself can have a significant impact on mental health.
Physical treatments for acne
• Light cautery/hyfrecation of macrocomedones: The tips of comedones are opened using a heat source which prevents the clogging of the follicles.
• Lasers/light-based devices – poor evidence to date.
• Chemical peels-remove comedones/ treat superficial scarring and hyperpigmentation – limited evidence.
Scarring in acne
Acne, especially severe acne, can cause scarring, which can be of two types:
Atrophic scarring where the skin is indented; eg , ice-pick scars (see Figure 4A).
Keloid scarring is raised off the skin (see Figure 4B).
Atrophic scars can be treated with resurfacing lasers such as fraxel or carbon dioxide lasers, whereas keloid scars may be treated with intralesional triamcinolone to flatten the scars.


Resources
For more information on acne, visit the acne support page on the Irish Skin Foundation website: https://irishskin.ie/acne/
Also, download the Irish Skin Foundation acne booklet What you need to know about acne at https://irishskin.ie/wp-content/uploads/2022/11/ISF-Acne-Booklet.22.11.2022.pdf
For acne (and many other skin conditions) support or guidance, visit the Founation’s Ask a Nurse resource at https://irishskin.ie/ask-our-dermatology-nurse/











Leave a Reply
You must be logged in to post a comment.