There is an urgent need for implementation of VTE prevention policies in Irish hospitals
Venous thromboembolism (VTE) continues to represent a major cause of cardiovascular death in developed countries, accounting for more deaths annually than road traffic accidents, retroviral disease, breast cancer and prostate cancer combined. While the pathophysiology of VTE is clearly complex and multi-factorial, recent evidence suggests that a feature which is common to a significant proportion (if not the majority of VTE cases) is recent admission to hospital. Moreover, there is also now evidence to suggest that by taking specific steps to identify high-risk hospital patients and by implementing VTE prevention measures where appropriate, that a significant proportion of these VTE events can be avoided and that lives can be saved.
Interestingly, while the development of novel treatment strategies for VTE has been a major focus of interest for clinicians in recent years, (particularly with the advent of the direct oral anticoagulants and interventional approaches to acute VTE therapy), the importance of VTE prevention in the first instance is often over-looked. The reason for this lack of focus on VTE prevention is likely to be multi-factorial. In Ireland the lack of high-quality epidemiological data relating to VTE incidence patterns likely contributes to the lack of awareness of VTE risk among staff on our hospital wards. Similarly, the lack of robust data collection tools limits our ability to identify high-risk groups within our healthcare system, to accurately audit practice or to measure our own performance in attempting to address this major healthcare risk. However, given the strong data demonstrating the life-saving effects of relatively simple, low-cost prevention measures (such as using standardised VTE risk assessment tools and mechanical/pharmacological thromboprophylaxis), it is clearly now a challenge for all clinicians engaged in hospital medicine to explore means of reducing VTE risk for their patients in collaboration with healthcare colleagues across the Irish healthcare system.
VTE: The global perspective
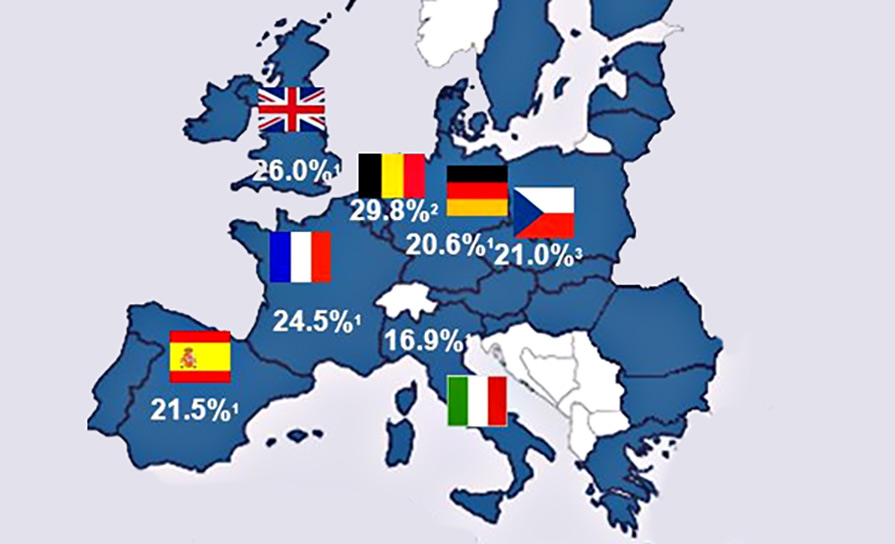
VTE, which comprises of deep vein thrombosis (DVT) and pulmonary embolism (PE), has been reported to occur at an incidence of approximately one per 1,000 adults per annum in the developed world. It is the third leading cause of cardiovascular death globally after myocardial infarction and stroke and has been estimated to account for over half a million deaths in Europe annually. Among individuals who present with a first episode of PE, the case fatality rate has been estimated as being at least as high as 10 per cent (and likely to be higher among certain high-risk groups including patients with cancer).
Among survivors, the chronic sequelae of VTE are often associated with a significant impact on quality of life and substantial healthcare costs. Common complications such as post-thrombotic syndrome (a complication of DVT characterised by chronic pain, swelling and skin ulceration in affected limbs) and chronic thromboembolic pulmonary hypertension have been reported to affect over 400,000 individuals in Europe every year. The healthcare resource burden associated with these long-term conditions, as well as the costs of acute VTE therapy, is considerable.
The pathophysiology of VTE disease is complex and multi-factorial. There are certainly a number of factors which clearly induce a prothrombotic state by various mechanisms and are associated with a significant VTE risk (eg, active cancer, pregnancy, major surgery). Interestingly, there are a number of other risk factors which are quite prominent in terms of the awareness among healthcare professionals and the general public, despite only conferring a very modest increase in baseline VTE risk (eg, long-haul travel, heterozygosity for common genetic polymorphisms such as factor V Leiden). Conversely, the very substantial risk of VTE associated with hospital admission (up to 100-fold from baseline) is often overlooked by patients and hospital staff alike.
Recent international data suggests that 50 per cent or more of all VTE events are hospital acquired (HA-VTE), which is defined as a VTE event occurring during hospital admission or within 90 days of discharge. Taking this finding into consideration, it would stand to reason that if it were possible to target VTE prevention strategies towards the group of individuals who make up the population comprising of hospital in-patients and recently discharged patients, that the overall global burden of VTE (including potentially fatal VTE events) could be reduced. Indeed, this hypothesis has been proven to be correct by counterparts in other healthcare systems including in the UK, where the implementation of mandatory VTE risk prevention strategies (with financial penalties for hospital trusts that fail to reach specific targets) has resulted in a significant reduction in HA-VTE and HA-VTE-related mortality.
Importantly, up to 50 per cent of all HA-VTE has been reported as occurring in the 90 days following hospital discharge. The optimum duration of pharmacological thromboprophylaxis required to reduce this persisting risk remains a source of considerable debate with recent clinical practice guidelines issued by the UK National Institute for Health and Care Excellence (NICE) recommending thromboprophylaxis for a minimum of seven days in at-risk patients even if this may require a number of days of treatment following hospital discharge. Many institutions favour a pragmatic approach with thromboprophylaxis continued for the duration of inpatient stay only (except for certain high-risk groups). The appropriate minimum duration of thromboprophylaxis is currently the subject of ongoing clinical research.
The Irish perspective
Currently data relating to patterns of VTE incidence are largely lacking within the Republic of Ireland. Unlike in the UK and other jurisdictions, there is no mandatory requirement to implement VTE prevention strategies at hospital level and therefore the use of VTE risk assessment tools and standardised guidelines directing use of pharmacological thromboprophylaxis tends to be implemented on an ad hoc basis.
The lack of VTE incidence data (and in particular HA-VTE incidence data) in Ireland and our current inability to collect data in a manner which would allow us to link new VTE events to any potential preceding hospital admission episode has likely contributed to our failure to clearly demonstrate the true magnitude of the VTE risk associated with hospital admission in this country. When VTE occurs in these ‘post-discharge’ cases, the causal association with the earlier hospital admission may sometimes not be readily apparent – in some cases the patient may present to a different hospital or be admitted under a different service. In some cases, the VTE event may be fatal (and perhaps only confirmed on autopsy – or not at all). Therefore, the impact of hospital admission or the impact of failing to implement VTE prevention measures (if applicable) might not always be apparent to healthcare staff or policy makers. This difficulty in capturing HA-VTE as a specific entity also hinders our ability to monitor our performance in reducing VTE at hospital and national level, a key factor in motivating staff and in influencing healthcare policy makers.
However, in recent years, the importance of prevention of HA-VTE has gained more prominence and through collaboration among healthcare providers, more and more institutions are striving to implement VTE prevention policies for patients admitted to hospital. In some institutions, VTE risk assessment tools and prescribing guidelines are being incorporated into hospital drug kardexes or being made freely available online in hospital intranets or in other readily accessible formats. In other institutions where electronic hospital records (EHR) have become established, a reminder to complete a VTE risk assessment (which requires an acknowledgement from the prescribing doctor prior to proceeding any further with patient documentation) has also been trialled. However, the implementation of such measures is not currently mandatory for individual hospitals and there are likely to be many institutions which lack a standardised VTE prevention policy.
Within the Ireland East Hospital Group (IEHG), which is the largest Irish hospital group, a VTE working group was established in May 2017 with the aim of promoting VTE awareness and standardising VTE treatment and prevention pathways across the group. This working group, comprising of representatives from all 11 of the IEHG hospitals as well as a representative from the patient advocacy group Thrombosis Ireland, have recently completed an observational study which aimed to determine the incidence of VTE and specifically HA-VTE within an entire hospital group. This study was unique for Ireland not only for the size of the population being studied (the population of the IEHG catchment area during the period of the study was calculated at 1,036,279 based on 2016 census data) but also incorporated data from large, tertiary academic centres (Mater Misericordiae University Hospital and St Vincent’s University Hospital) as well as the National Maternity Hospital, Cappagh National Orthopaedic Hospital, several regional hospitals and included data from contrasting sociodemographic regions. The results of this study, recently published in BMJ Open, reflect the patterns of VTE incidence which have been reported in other similar populations outside of Ireland. In total, 2,727 VTE events were reported within the catchment area of the IEHG during the 22-month study period, corresponding to an annual VTE incidence of 1.44 per 1,000. Within the limitations of the data collection methodology, the proportion of HA-VTE events was estimated at 47 per cent although this was likely to have been a significant underestimation given the inability of current data collection tools to link VTE diagnostic codes to recent inpatient episodes for the patients with HA-VTE who presented with their VTE event shortly following discharge. The majority of the HA-VTE events were reported as occurring in the context of an emergency hospital admission and the most frequent groups of patients affected with HA-VTE were patients admitted with a cancer diagnosis, cardiovascular disease or respiratory disease. As expected, the incidence of VTE in general within the group increased with increasing age.
The future of VTE prevention in Ireland
In July 2018, the HSE Quality Improvement Division published the Preventing blood clots in Hospitals report and National Guidelines. As well as demonstrating the dramatic improvements in rates of appropriate use of thromboprophylaxis, which can be achieved through education and collaborative learning, this report also set out a number of recommendations on how measures can be taken in our hospitals to reduce the risk of HA-VTE. In particular, this report recommends that all patients admitted to hospital undergo a VTE risk assessment as soon as possible following admission and that, where indicated, mechanical/pharmacological thromboprophylaxis is administered. As we have reported recently from the IEHG, the incidence of HA-VTE in Ireland appears to at least match that seen in other developed countries. In these other countries, the majority of HA-VTE have been shown to be preventable using standardised VTE risk assessment tools and thromboprophylaxis. Moreover, the implementation of these relatively simple and low-cost measures have been shown to save lives. Therefore, taking into account the HSE recommendations, international data and our own attempts to describe VTE incidence patterns in Ireland, healthcare providers in this country must now look to addressing this important cause of hospital deaths in a systematic and sustained manner. With the support of agencies such as the HSE and patient advocacy groups such as Thrombosis Ireland, the potential for collaboration between clinicians and other stakeholders at Hospital Group, in the community, and at national level is increasing and therefore implementing safe and effective strategies in all hospitals across this country in order to address the serious risk of HA-VTE must now be recognised as an urgent and achievable goal.
References on request
VTE Dublin is a not for profit annual conference held in Dublin every Autumn, which offers the cutting edge in what is happening and what is coming in VTE. It is organised by a multidisciplinary group of clinicians passionate about improving VTE care both locally and internationally. VTE Dublin 2019 was the group’s fifth conference. Attendance has grown from strength to strength and the meeting has attracted many of the world leaders in VTE care and research. As well as a varied programme of speakers covering topics such as VTE in pregnancy, managing anticoagulation patients, and cancer-associated thrombosis, the conference hosts an annual point of care ultrasound workshop dedicated to VTE. This year’s conference, entitled ‘VTE Dublin 2019 – Diagnostic and therapeutic advances in venous thromboembolism (VTE)’, took place from 25 to 27 September in the Hogan Mezzanine Suite, Croke Park and the Mater Misericordiae University Hospital, Dublin. For full details see www.vtedublin.org.
Fast facts on VTE:
One-in-four people will die of causes related to blood clots.
More people die each year from blood clots than from breast cancer, prostate cancer, and road traffic accidents combined.
Blood clots are reported to be potentially the number one cause of preventable death in hospital ahead of infection and pneumonia according to international data.
Over half of all cases are as a direct result of a hospital stay.
VTE is one of the leading causes of maternal death in the UK and Ireland.
All pregnant women should have a VTE risk assessment when they book, when they deliver and if risk factors change.
Women starting HRT or hormonal contraception should have a conversation with their doctor around their personal risk factors, such as family or personal VTE history.
There are 5,000 cases of VTE in Ireland each year (of which over half are estimated to be hospital-acquired), and many are preventable.
For further information on VTE go to www.ThrombosisIreland.ie










Leave a Reply
You must be logged in to post a comment.