Priscilla Lynch reports on the latest positive findings regarding HIV treatment and prevention
Earlier this month, a major international study published in The Lancet provided conclusive evidence that the risk of HIV transmission through sex when HIV viral load is suppressed is effectively zero, and made international headlines. The findings support the message of the U=U (undetectable equals untransmittable) campaign, and the benefits of early testing and treatment for HIV.
The PARTNER study was a prospective observational study carried out at 75 sites in 14 European countries. Between Sept 15, 2010, and July 31, 2017, 972 gay male couples were enrolled in the PARTNER2 study, of which 782 provided 1,593 eligible couple-years of follow-up, with a median follow-up of two years. At baseline, median age for HIV-positive partners was 40 years and couples reported condomless sex for a median of one year. Unlike other studies on HIV transmission, this study only recruited couples that had already chosen not to use condoms and in the primary analysis, researchers only included periods when condoms were not used and with no use of pre-exposure prophylaxis (PrEP) or post-exposure prophylaxis (PEP) by the HIV-negative partner.
During eligible couple-years of follow-up, couples reported condomless anal sex a total of 76,088 times. A total of 288 (37 per cent) of 777 HIV-negative men reported condomless sex with other partners. Just 15 new HIV infections occurred during eligible couple-years of follow-up, but none were phylogenetically linked within-couple transmissions, resulting in a HIV transmission rate of zero (upper 95 per cent CI 0•23 per 100 couple-years of follow-up).
The researchers estimated that, based on the type and frequency of sexual contact, effective treatment prevented around 472 HIV transmissions.
The findings provide a level of evidence on viral suppression and HIV transmission risk through condomless sex for gay men similar to that already reported for heterosexual couples; indicating that the risk of HIV transmission when HIV viral load is suppressed is effectively zero for both anal and vaginal sex. This is important because without a positive partner being on treatment, anal sex is at higher risk for HIV transmission compared to vaginal sex.
The study authors said the results from the PARTNER studies support wider dissemination of the message of the U=U campaign, to promote the benefits of early testing and treatment and to tackle stigma, discrimination, and criminalisation laws that continue to affect HIV-positive people.
However, a sustained effort is required to increase rates of testing and HIV diagnosis with early initiation of antiretroviral therapy (ART) and full support to maintain high levels of adherence, the study authors note.
Lead author Prof Alison Rodger (University College London Institute for Global Health and Royal Free London NHS Foundation Trust) said: “Our findings support the message of the international U=U campaign, that a suppressed viral load makes HIV untransmittable. This message has been endorsed by more than 780 HIV organisations in 96 countries and can help end the HIV pandemic by preventing HIV transmission and tackling the stigma and discrimination that many people with HIV face.
“Increased efforts must now focus on wider dissemination of this powerful message and ensuring that all HIV-positive people have access to testing, effective treatment, adherence support and linkage to care to help maintain an undetectable viral load.”
Also commenting, Dr Michael Brady, Medical Director at the Terrence Higgins Trust, said: “It is impossible to overstate the importance of these findings.
“The PARTNER study has given us the confidence to say, without doubt, that people living with HIV who are on effective treatment cannot pass the virus on to their sexual partners.
“This has incredible impact on the lives of people living with HIV and is a powerful message to address HIV-related stigma.” So while there remains no time-limited treatment full ‘cure’ for HIV, its end could be in sight, once all those infected are initiated on treatment.
However, in 2017, there were almost 40 million people worldwide living with HIV, of whom just over half, 21.7 million, were on ART.
Ireland
The Health Information and Quality Authority (HIQA) recently launched a public consultation on a draft health technology assessment (HTA) of a PrEP programme for populations at substantial risk of sexual acquisition of HIV in Ireland.
The report confirms PrEP is safe and highly effective at preventing HIV in people at substantial risk, and also finds that the introduction of a PrEP programme would be cost-saving.
PrEP essentially involves the pre-emptive use of oral ART in HIV-negative people to prevent infection. PrEP consists of a fixed-dose combination of oral tenofovir/emtricitabine and has been licensed for use in Ireland since 2016. A ‘PrEP programme’ provides PrEP as part of a holistic service that includes frequent monitoring for adherence and side-effects, testing for HIV and other STIs, and counselling and advice on safer sex practices.
HIQA’s Director of Health Technology Assessment and Deputy Chief Executive, Dr Máirín Ryan, said: “HIV infection remains a significant public health concern. There were 492 diagnoses of HIV notified in Ireland in 2017. Just over half of all notifications were in men who have sex with men.”
She said that from reviewing the evidence, HIQA has found that PrEP is safe and highly effective at preventing HIV in people at substantial risk. Additionally, implementing a PrEP programme would be considered cost-saving compared with standard care.
“The effectiveness of PrEP is strongly linked with taking the medication correctly, and PrEP must not be taken by individuals with an unrecognised HIV infection, as drug resistance mutations may develop. This means that it is important that people taking part in a PrEP programme should receive advice on taking the medication appropriately and undergo frequent HIV testing.”
Following the consultation process, a final report will be prepared for consideration by the HIQA Board. The completed assessment will be submitted to the Minister for Health and the HSE and published on the HIQA website.
Taoiseach Leo Varadkar TD and Minister for Health Simon Harris both welcomed the publication of HIQA’s draft report on the introduction of a PrEP programme aimed at preventing HIV.
Commenting, Minister Harris said: “Reducing the number of new HIV diagnoses in Ireland is a priority focus for me as Minister for Health. The introduction of a PrEP programme will make a significant contribution to that aim.”
The Minister continued: “As the report notes, many of the people who would stand to benefit from a PrEP programme are from vulnerable or stigmatised groups in our society, so it is important that we continue to work to reach out and encourage more people to get tested and avail of the treatments and supports available.
“Considerable work is already underway in the HSE to prepare for the introduction of a PrEP programme that meets appropriate standards. I encourage interested parties and members of the public to give their feedback on the draft report during the consultation process, which runs to 28 May, and I thank HIQA and the various experts and stakeholders for their work so far. I look forward to receiving HIQA’s formal advice when the report is finalised after the consultation process.”
HIV drug resistance in Ireland — improving prevalence estimates
HIV antiviral drugs are at risk of becoming ineffective due to emerging HIV drug resistance. Transmitted drug resistance (TDR) occurs in people who have never previously taken antiretroviral therapy (ART) and is of serious public health concern due to implications at both the individual and population level. At an individual level, persons with TDR begin ART with a lower genetic barrier to resistance and a higher risk of virological failure. At a population level, TDR significantly impacts national treatment guidelines and first-line treatment options. As such, the World Health Organisation (WHO) recommends population surveillance of TDR, both in order to preserve ART options, and to control future HIV epidemics.
Under the guidance of a multidisciplinary, multisectoral steering group, including the Health Protection Surveillance Centre (HPSC), UCD National Virus Reference Laboratory (NVRL), public health clinicians, HIV Ireland, and Positive Now, data were analysed from individuals diagnosed with HIV-1 in Ireland during 2017. For the first time epidemiological data on prior ART, using the national Computerised Infectious Disease Reporting System (CIDR), were linked with drug resistance data from the NVRL, to improve the accuracy of the estimates.
A report published in April 2019 by the HPSC and NVRL shows that the prevalence of HIV TDR among people diagnosed with HIV in 2017 was 9 per cent.
Individuals were determined to have TDR if they were ART-naïve and were detected with a least one surveillance drug resistance mutation (SDRM) from the WHO SDRM list.
Of 283 individuals tested, 16 were detected with SDRM; 13 with single-drug class resistance, and three with dual-class resistance. The prevalence of TDR to any drug class was 9 per cent, ie, 16 people.
By drug class, the prevalence of non-nucleoside analogue reverse transcriptase inhibitor (NNRTI) TDR (8 per cent; n=14) was higher than nucleoside-analogue reverse transcriptase inhibitor (NRTI) TDR (1 per cent; n=2) and protease inhibitor TDR (2 per cent; n=3). No individuals were identified to have integrase inhibitor-resistant virus.
The prevalence of TDR was higher among some at-risk groups, in particular migrants from countries in sub-Saharan Africa (13 per cent), and men who have sex with men (MSM) (9 per cent).
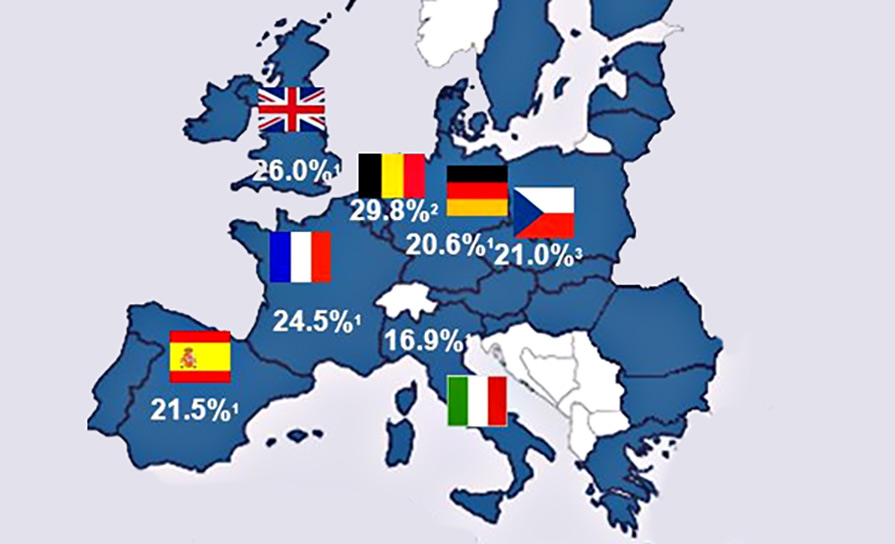
European-level TDR surveillance by the European Centre for Disease Prevention and Control is due to commence in 2019, and will add valuable context to the Irish results, which will help to inform the management of HIV in Ireland.
Source: HPSC Epi-Insight, volume 20, issue 5.










Leave a Reply
You must be logged in to post a comment.