Both oral and genital herpes are mostly asymptomatic or unrecognised, but can cause painful blisters and ulcers, with more severe impacts in the immunocompromised
The herpes simplex virus (HSV), more commonly known as herpes, is categorised into two types: HSV-1 and HSV-2. Both are members of the Herpesviridae family, a group of double-stranded enveloped DNA viruses that cause various infections and certain diseases, and include Varicella Zoster virus (VZV), Cytomegalovirus (CMV), Epstein-Barr virus (EBV) and Human Herpesvirus (HHV) 6, 7, and 8, which are common among humans.2
HSV-1 is mainly transmitted via contact with the virus in sores, saliva or surfaces in or around the mouth and causes oral herpes (cold sores). HSV-1 can also be transmitted to the genital area through oral-genital contact and cause genital herpes. Oral herpes infection is mostly asymptomatic, but symptoms can include painful blisters or open sores in or around the mouth. Infected persons will often experience a tingling, itching or burning sensation around their mouth before the appearance of sores. These symptoms can recur periodically, and the frequency varies from person to person.1
HSV-2 is a sexually transmitted infection that causes genital herpes. HSV-2 is mainly transmitted through contact with genital or anal surfaces, skin, sores or fluids of a person infected with the virus. HSV-2 can be transmitted even if the skin looks normal, and is often transmitted in the absence of symptoms.1
An estimated 3.7 billion people under the age of 50 years (67 per cent) have HSV-1 infection globally, and an estimated 491 million people aged 15-to-49 years (13 per cent) worldwide have HSV-2 infection (WHO 2016 last available estimates). Infection with HSV-2 increases the risk of acquiring and transmitting HIV infection.1
Genital herpes can be caused by HSV-1 or HSV-2 and manifests as either a primary or recurrent infection. Most commonly, viral replication occurs in epithelial tissue and establishes dormancy in sensory neurons, reactivating periodically as localised recurrent lesions.HSV remains one of the most common STIs, but continues to be under-identified, given the vague presentation of its symptoms. When symptoms occur, genital herpes is characterised by one or more genital or anal blisters or ulcers. Symptoms of a new infection often include fever, body aches and swollen lymph nodes. After an initial episode, which can be severe, symptoms may recur. Genital herpes caused by HSV-1 mtypically does not recur frequently, but with HSV-2 infection, recurrent symptoms are common. However, recurrences are often less severe than the first episode and tend to decrease over time.1,2
Risk factors
Risk factors for HSV-1 infection differ depending on the type of HSV-1 infection. In the case of orolabial herpes (cold sores), risk factors include any activity that exposes an individual to an infected person’s saliva. A risk factor for herpetic sycosis includes close shaving with a razor blade in the presence of an acute orolabial infection. Risk factors for herpetic whitlow include thumb sucking and nail biting in the presence of orolabial HSV-1 infection in children, although HSV-2 most commonly causes herpetic whitlow in adults.5
Risk factors for acquiring HSV-2 infection involve direct exposure to fluids from a seropositive individual containing viral products, most often during sexual intercourse. HSV-2 is mainly transmitted through sexual intercourse, attributing to its predominant rise starting at puberty. Both primary and recurrent HSV infections in pregnant women can lead to intrauterine transmission and resultant congenital HSV infection.2
Pathophysiology
HSV-1 is typically spread through direct contact with contaminated saliva or other infected bodily secretions, as opposed to HSV-2, which is primarily spread by sexual contact. HSV-1 begins to replicate at the site of mucocutaneous infection and then proceeds to travel by retrograde flow down an axon to the dorsal root ganglia (DRG), where latency is established. The latency period allows the virus to remain in a non-infectious state for a variable amount of time before reactivation.2
HSV-2 is transmitted through direct contact of secretions in a seropositive individual who is actively shedding the virus. The virus affects the skin and mucous membranes invading epithelial cells on initial exposure, and ultimately replicating intracellularly at that site. After initial exposure the symptoms resolve in 10-to-14 days, but the virus lies dormant in the periaxonal sheath of the sensory nerves of either the trigeminal, cervical, lumbosacral, or autonomic ganglia. In these locations, viral replication is often controlled by the patient’s immune system and remains in a dormant state only to reactivate later in life. When reactivation occurs, the virus travels through the sensory nerves until it reaches the mucocutaneous sites where replication takes place, and leads to vesicular clusters at the dermatological site of that sensory neuron.2
Complications
HSV-2 infection increases the risk of acquiring HIV infection. People with both HIV and HSV-2 infection are more likely to spread HIV to others. HSV-2 infection is among the most common infections in people living with HIV. In immunocompromised people, including those with advanced HIV infection, herpes can have more severe symptoms and more frequent recurrences.1
Rare complications of HSV-2 include meningoencephalitis and disseminated infection. Rarely, HSV-1 infection can lead to more severe complications such as encephalitis or keratitis. Ocular HSV is a common cause of blindness when it manifests as keratitis or a branching dendritic corneal ulcer.1,5
Neonatal herpes can occur when an infant is exposed to HSV during delivery. Neonatal herpes is rare, occurring in an estimated 10 out of every 100,000 births globally. However, it is a serious condition that can lead to lasting neurologic disability or death. The greatest risk for neonatal herpes is when a mother acquires primary genital herpes in the third trimester of pregnancy, especially within six weeks of delivery, as the neonate will be unlikely to have acquired protective antibodies in this time.1
HSV remains one of the most common sexually-transmitted infections but continues to be under-identified, given the vague presentation of its symptoms
Presentation and diagnosis
The major clinical manifestations of infection with HSV-1 or HSV-2 are oral, genital, and ocular ulcers. Less commonly, primary or recurrent HSV infections may also present at other sites with neurological, hepatic, or respiratory complications. The primary episode occurs during initial infection with HSV, in which the host lacks an antibody response.8
HSV-1 infection is frequently asymptomatic. When symptoms do occur, there is a wide range of clinical presentations that can occur including orolabial herpes, HSV folliculitis, herpes gladiatorum, herpetic whitlow, ocular HSV infection, herpes encephalitis, Kaposi varicelliform eruption (eczema herpeticum), and severe or chronic HSV-1 infection.5 HSV-1 is the most common cause of orolabial herpes. When symptoms occur, the most common manifestation is a ‘cold sore’ on the mouth/lips.5
In children, symptomatic orolabial HSV-1 infections can present as gingivostomatitis that leads to pain, halitosis, and dysphagia. In adults, it can present as pharyngitis and a mononucleosis-like syndrome.5 Symptoms of a primary orolabial infection occur between three days and one week after exposure. Patients will often experience a viral prodrome consisting of malaise, anorexia, fever, tender lymphadenopathy, localised pain, tenderness, burning, or tingling prior to the onset of mucocutaneous lesions. Primary HSV-1 lesions usually occur on the mouth and lips. Symptoms of recurrent orolabial infection are typically milder than those of primary infection, with a 24-hour prodrome of tingling, burning, and itch. Recurrent orolabial HSV-1 infections classically affect the vermillion border of the lip, as opposed to the mouth and lips as seen in primary infection.5
Genital herpes can be caused by either HSV-1 or HSV-2. HSV-2 may present as a primary infection with painful genital ulcers, sores, crusts, tender lymphadenopathy, and dysuria. The classical features are of macular or papular skin and mucous membrane lesions, progressing to vesicles and pustules that often last for up to three weeks. Genital lesions can be especially painful, leading to swelling of the vulva in women, burning pain, and dysuria. Systemic symptoms can include fever, headache, and malaise and are often due to concurrent viraemia.2
Diagnosis can be made clinically, but should be confirmed with an HSV NAAT swab of the lesions to determine if the cause is HSV-1 or HSV-2. If there is no obvious active infection, a HSV antibodies blood test may be carried out to screen for the virus. The HSV antibodies test is not as reliable as culturing a sample, but can help identify the recurrence of a previous infection.8
As HSV-2 is an STI, individuals diagnosed with genital herpes should be offered testing for other STIs including HIV, hepatitis B, syphilis, chlamydia, and gonorrhoea. Testing for hepatitis C should be considered part of routine sexual health screening in men who have sex with men (MSM); people living with HIV; commercial sex workers; and people who inject drugs (PWID). Partners should also be considered for HCV testing.4
Pregnant women with a history of genital herpes should inform their obstetrician and referral to a GUM clinic should be considered, particularly if the patient is experiencing frequent recurrences. Patients presenting with genital herpes for the first time in pregnancy should have the diagnosis confirmed, treatment started, and be referred to a GUM clinic. Patients presenting with frequent recurrences (>/= one per month) should be offered suppressive therapy and may be best managed at a GUM clinic. Genital herpes is a notifiable disease.4
Treatment
Although there is no cure for HSV, treatments can relieve the symptoms. Medication can decrease the pain related to an outbreak, shorten healing time, and can also decrease the total number of outbreaks. Antiviral drugs including acyclovir, famciclovir, and valacyclovir, are among the medications used to treat the symptoms of herpes. If given within 72 hours of symptom onset, antivirals can be effective in reducing the severity and duration of symptoms, however, early treatment of primary infection does not prevent recurrences.1,3
Infection with HSV-2 increases the risk of acquiring and transmitting HIV infection
Treatment of genital herpes
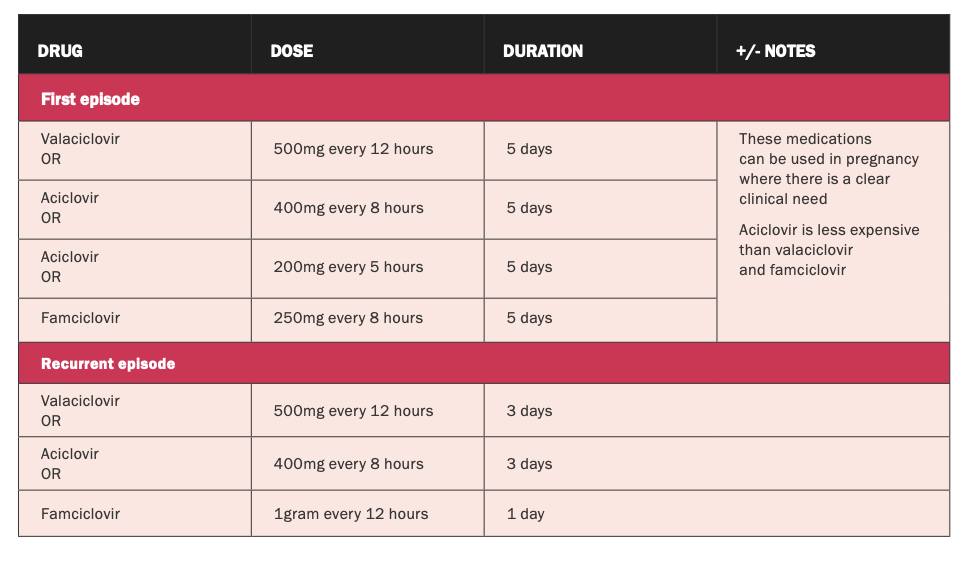
Treatment should be started based on clinical impression (See Table 1).4 Goals are to treat and prevent symptomatic genital herpes recurrences, and prevent transmission to sexual partners by supressing the virus.6
- Topical antiviral medication is not as effective as oral antiviral medication.
- Simple oral analgesia, eg, ibuprofen or paracetamol, and local anaesthetic cream, eg, EMLA cream.
- Warm baths may help relieve the pain associated with genital sores.
- Hospitalisation may be required for urinary retention, meningism or severe constitutional symptoms.4
The latest HSE prescribing guidance on genital herpes is available at: www.hse.ie/eng/services/list/2/gp/antibiotic-prescribing/conditions-and-treatments/genital/genital-herpes/genital-herpes.html.
Prevention
People with symptoms of oral herpes should avoid oral contact with others, including oral sex and sharing objects that touched saliva. Individuals with symptoms of genital herpes should abstain from sexual activity while experiencing symptoms. Both HSV-1 and HSV-2 are most contagious when sores are present, but can also be transmitted when no symptoms are felt or visible. For sexually-active people, consistent and correct use of condoms is the best way to prevent genital herpes and other STIs. However, HSV infection can still occur through contact with genital or anal areas not covered by the condom. People with symptoms suggestive of genital herpes should be offered HIV testing. Pregnant women with symptoms of genital herpes should inform their healthcare providers. Preventing acquisition of HSV-2 infection is particularly important for women in late pregnancy when the risk for neonatal herpes is greatest.1,3
Prognosis
Once a person contracts HSV, it is a lifelong condition. There is no cure. Overall, most HSV-1 infections are asymptomatic, and if symptomatic; present with mild recurrent mucocutaneous lesions. The prognosis of HSV-1 infection varies depending on the manifestation and location of the HS-1 infection. Early identification of symptoms and prompt use of pharmacotherapy can lead to early suppression of viral replication. The key to treatment is starting the antiviral within 24 hours of symptoms. Abstinence from sex during known viral shedding can decrease the risk of transmission to a seronegative partner. The herpes viruses
as a family are responsible for significant neurological morbidity, and HSV-2 persists in the seropositive individual for a lifetime.2
Vaccinations
HSV vaccines are being researched and studied to reduce the severity of symptoms and help expedite visible lesion healing. By reducing shedding, severity may be reduced, as has been seen with the Varicella-zoster vaccination. HSV vaccines are being researched and developed with two broad focuses; preventative and therapeutic, and some with a dual use as both immunotherapeutic and prophylactic.7 Although several candidate HSV vaccines are in the pre-clinical and clinical phases of study and have been tested in humans, there are currently no licensed vaccines available against either HSV type.
References
WHO (2022). Herpes simplex virus. World Health Organisation, Geneva. Available at: www.who.int/news-room/fact-sheets/detail/herpes-simplex-virus
Jacob M (2022). Herpes Simplex type 2. StatPearls Publishing. Available at: www.statpearls.com/ArticleLibrary/viewarticle/688
WebMD (2022). Herpes simplex virus: HSV-1 and HSV-2. Available at: www.webmd.com/genital-herpes/pain-management-herpes#1
HSE (2021). Genital herpes. Available at: www.hse.ie/eng/services/list/2/gp/antibiotic-prescribing/conditions-and-treatments/genital/genital-herpes/genital-herpes.html
Saleh D, Yarrarapu S, Sharma S (2022). Herpes simplex type 1. StatPearls Publishing. Available at: www.ncbi.nlm.nih.gov/books/NBK482197/
MIMS (2022). Herpes simplex virus infections. Available at: https://specialty.mims.com/herpes%20simplex%20virus%20infection/treatment
WHO (2022). Herpes simplex virus. World Health Organisation: Immunisation, vaccines and biologicals. Available at: www.who.int/teams/immunization-vaccines-and-biologicals/diseases/herpes-simplex-virus
BMJ (2022). Herpes Simplex Virus Infection. BMJ Best Practice. Available at: https://bestpractice.bmj.com/topics/en-gb/53











Leave a Reply
You must be logged in to post a comment.