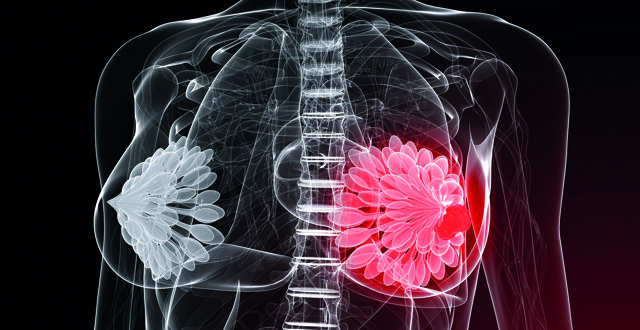
Breast cancer is the commonest, potentially fatal cancer diagnosed in women in Ireland, according to the latest National Cancer Registry Ireland (NCRI) statistics. The median age at diagnosis is 60 – 64 years. Women under the age of 40 have an incidence of 11.93 diagnoses per 100,000 women per year. This patient population poses specific challenges and here we attempt to address some of these, namely pregnancy-associated breast cancer, optimum adjuvant endocrine treatment, fertility post-treatment and inherited breast cancer syndromes.
<h3 class=”subheadMIstyles”>Pregnancy-associated breast cancer</h3>
Pregnancy-associated breast cancer is defined as breast cancer diagnosed during pregnancy or in the first postpartum year. With most pregnancies occurring in women under the age of 40 years, it is this age group that is at risk of pregnancy-associated breast cancer. The incidence of breast cancer increases with age and as increasing numbers of women delay pregnancy, it is possible that pregnancy-associated breast cancer will increase. Several studies have indicated a worse prognosis in those with pregnancy-associated breast cancer; these cancers tend to have higher T and N stages. Even allowing for this, some studies have demonstrated worse cancer-related outcomes for those with pregnancy-associated breast cancer.
No statistics are available at present for the incidence in Ireland, but it is estimated that approximately one-in-3,000 pregnant women will be diagnosed with breast cancer, making it the second most common malignancy in pregnancy. Several challenges arise in this setting, including difficulties in diagnosis, optimum timing of surgery, scheduling of systemic treatment and maximising neonatal outcomes. The Royal College of Obstetrics and Gynaecology recommends that all women presenting with a breast mass during pregnancy be referred for evaluation to a specialist breast unit. Surgery is safe during all stages of pregnancy, but should be delayed until after the first trimester, when the risk of miscarriage diminishes. Radiation is not recommended for patients who are pregnant. Cytotoxic chemotherapy use is generally initiated in the second trimester, with evidence for good neonatal outcomes with the use of anthracycline/cyclophosphamide combinations. Due to the risk of oligohydramnios, trastuzumab is not given during pregnancy. In general, cytotoxic chemotherapy is held at 35 weeks to reduce the risk of neonatal neutropaenia. Endocrine therapy is not given until after delivery.
<h3 class=”subheadMIstyles”>Optimum adjuvant endocrine treatment</h3>
Tamoxifen is a selective oestrogen receptor modulator and has been a mainstay of treatment for women with oestrogen receptor-positive breast cancer for decades. Its use has been refined over this time, with it now being used primarily in pre-menopausal women. However, even with five years of adjuvant tamoxifen therapy, some patients will relapse and so strategies to optimise adjuvant endocrine treatment in patients have been further explored. Such strategies include prolonging the duration of therapy or more aggressive suppression of hormonal function.
Two large multicentre randomised studies evaluated the utility of extended tamoxifen therapy, beyond the standard five years, ATLAS and ATTOM. Initial results of both studies suggested that there was no survival benefit to this therapy. Follow-up survival data, however, demonstrated a benefit to extended adjuvant tamoxifen, which appeared after the 10-year period of treatment and, therefore, this is a potential therapeutic strategy for these patients. Such a prolonged course of therapy might be best targeted at patients with a persistent elevated risk of relapse after five years of therapy, eg, those patients with pathologically involved lymph nodes at diagnosis.
Two other large studies have evaluated the optimum intensity of adjuvant endocrine treatment. The TEXT and SOFT studies sought to establish if further oestrogen suppression with triptorelin, a GnRH agonist, in combination with either exemestane (an aromatase inhibitor) or tamoxifen would improve survival. The TEXT study evaluated exemestane, a steroidal aromatase inhibitor, in combination with triptorelin, a GnRH agonist compared to tamoxifen and triptorelin. This trial demonstrated an improvement in disease-free survival in those patients on exemestane and triptorelin compared to tamoxifen and triptorelin. No overall survival benefit was seen. In the SOFT study, when compared to tamoxifen alone, tamoxifen and triptorelin demonstrated a 4 per cent disease-free survival benefit, with a 7 per cent disease-free survival benefit in those on exemestane and triptorelin. Unlike the TEXT study, an overall survival benefit was seen, largely coming from the higher risk group (those patients requiring adjuvant chemotherapy). There is, however, a higher adverse effect rate, with increased vasomotor symptoms, decreased libido, vaginal dryness, and musculoskeletal symptoms among others. Given the modest benefit, this combination approach is usually offered to those patients at higher risk of recurrence (especially very young patients, ie, those under 35 years of age).
<h3 class=”subheadMIstyles”>Fertility post-treatment</h3>
In younger breast cancer patients, preservation of fertility is often a key priority. There are several concerns at this time – preventing premature ovarian failure, timing of future pregnancies to maximise oncologic and fertility outcomes and the need to avoid teratogenicity with ongoing treatment.
Fertility preservation prior to embarking upon treatment can be considered in those patients who wish to do so. There are two main techniques that are available to patients: Oocyte or embryo preservation. Oocyte preservation requires a short cycle of stimulatory hormonal therapy, after which the oocytes are retrieved and rapidly frozen. In Ireland, embryo preservation is offered to those with a long-term partner. The first step is as for oocyte preservation, with subsequent fertilisation and embryos are then frozen. With modern oocyte stimulation techniques, delays to the initiation of chemotherapy can be kept to a minimum.
Administration of GnRH analogues during chemotherapy may help preserve ovarian function. A recent meta-analysis of the use of GnRH analogues, pooling the data from several international studies, demonstrated improved post-chemotherapy fertility. The authors classified this as (1) improved premature ovarian insufficiency rate (variously identified as failure to return to normal menstruation within six-24 months depending on the study), (2) higher pregnancy rate, and (3) reduced rates of amenorrhoea at two years. They did not find any evidence of excess cancer-related mortality in those who received the GnRH analogue. Thus, this provides a potential option for these patients.
Pregnancy post-breast cancer diagnosis poses challenges in treatment continuity and risks of recurrence. Data is sparse, but a recently reported retrospective study examining 1,200 patients did not demonstrate any increased risk of recurrence in those women who became pregnant post-early breast cancer diagnosis.
Timing of pregnancy can be a challenge. The risk of recurrent cancer in patients with triple negative and HER2-positive breast cancer is highest in the first two years after diagnosis and the advice for these women is generally to avoid pregnancy until this period has passed. The situation is more complex for those with oestrogen receptor-positive breast cancer. For these patients, adjuvant endocrine therapy is an essential part of treatment, with the goal of treatment being oestrogen suppression. However, tamoxifen is contraindicated in those planning a pregnancy due to the risk of teratogenicity. It is therefore recommended that such women stop tamoxifen for three months prior to attempting to conceive. The reduced duration of therapy may expose the patient to a higher risk of relapse and patients must be counselled on this risk.
Another factor to consider in the young woman post breast cancer diagnosis is the potential teratogenicity of therapies. As outlined in this article, cytotoxic treatments are carefully scheduled. Once commenced on adjuvant endocrine therapy, patients should be advised to use effective contraception. Available data on tamoxifen suggests there is a risk of congenital malformations and a three-month washout period is advised.
<h3 class=”subheadMIstyles”>Inherited breast cancer syndromes</h3>
When a young woman is diagnosed with breast cancer, the question of an underlying genetic predisposition often arises. Most cases of breast cancer are not caused by an identifiable inherited predisposition, instead having a multifactorial origin. However, 5-10 per cent of breast cancers can be attributed to a single gene mutation, which significantly increased the predisposition to cancer development. Between 80-90 per cent of all hereditary breast cancers are associated with mutations within the BRCA1 and BRCA2 genes, with less common syndromes including Li Fraumeni syndrome, Peutz-Jeghers syndrome, Cowden syndrome and ataxia/telangiectasia also causing an increased risk. To identify those at risk, a complete, three-generation family history must be obtained from patients. A complete discussion of the intricacies of each syndrome is beyond the scope of this article and we will focus on BRCA syndromes. Various testing platforms exist, ranging from those examining specific targets (such as in a family with a known BRCA mutation) and those offering panel testing, assessing risk associated with more than one syndrome.
BRCA1 and BRCA2 function as tumour-suppressor genes, playing a role in DNA repair and are inherited in an autosomal dominant fashion with incomplete penetrance. Testing for BRCA1/2 mutations should be performed in the context of pre- and post-treatment counselling. The Manchester Criteria are used to help determine which patients should be offered testing. Those patients who are found to be carriers can then discuss appropriate surveillance and potential risk-reducing procedures. More widespread population-based screening is considered in some centres. In this instance, BRCA1/2 testing is offered to all patients under 40 years, or all those with triple-negative breast cancer.
<h3 class=”subheadMIstyles”>In summary</h3>
Managing breast cancer in young women is a complex challenge, requiring balancing of multiple factors. When breast cancer complicates pregnancy, co-ordination between the oncologist and obstetrician is imperative to optimise outcomes. Close communication between all members of the multidisciplinary team helps to facilitate fertility preservation and genetic testing. The most recent data available offers several combination strategies to optimise adjuvant endocrine therapy for these patients.
<p class=”referencesonrequestMIstyles”><strong>References on request</strong>












Leave a Reply
You must be logged in to post a comment.