A detailed overview of the prevention, diagnosis, and management of diabetic foot disease.
Diabetic foot ulceration (DFU) is a vascular complication of diabetes mellitus and associated with extensive periods of hospitalisation and a high degree of morbidity and mortality. The pathogenicity of diabetic foot ulcers are multifactorial. Diabetic foot syndrome (DFS) is associated with neurologic abnormalities and peripheral arterial disease of the lower limbs of varied severity. DFS involves infection, ulceration, or destruction of deep tissues of the foot including bones in a patient with diabetes mellitus and is defined by the World Health Organisation (WHO) as an “ulceration of the foot (distally from the ankle and including the ankle) associated with neuropathy and different grades of ischemia and infection”
Diabetes mellitus is a disorder of glucose haemostasis, which causes hyperglycaemia. When high blood glucose levels persist, complications occur causing damage in the wall of blood vessels throughout the body systems. A combination of damage in both small and large blood vessels leads to the presence of DFS manifesting in DFU. Neuropathy and vascular abnormalities are involved in the development of DFS. The underlying cause of DFS is the complex interaction between large vessel disease causing peripheral arterial disease (PAD) and small vessel disease leading to peripheral diabetic sensory neuropathy.
Motor neuropathy results in atrophy of foot muscles, disturbing the flexor-extensor balance and leading to contractures. Sensory neuropathy including abnormal sensation of pain, temperature, and touch exposes the
patient to repeated uncontrolled injuries, increasing the risk of ulcerations. Autonomic neuropathy results in the formation of arteriovenous fistulae and trophic changes and atherosclerosis of the lower extremities results in foot ischaemia. All these changes are associated with the development of local osteoporosis and may also lead to osteomyelitis, avascular necrosis, fractures, dislocations, and Charcot foot arthropathy.
DFS affects nearly 6 per cent of individuals with diabetes, and round 0.5-to-1.5 per cent of patients with DFS require amputation. Most amputations start with ulcerations and can be prevented with good foot care and screening to assess the risk of foot complications. DFS is associated with neurologic abnormalities and peripheral arterial disease of the lower limbs of varied severity. All patients with diabetes should have an annual screen to identify their foot ulcer risk status. Those with any risk factors require specific foot care education as well as regular contact with a healthcare professional, usually a podiatrist. Most important in the identification of the high-risk neuropathic foot is good clinical observation and removal of the shoes and socks, with careful inspection of the feet as part of the routine follow up of all patients with diabetes.
Risk factors for developing diabetic foot ulcers
All people with diabetes are at risk of developing foot ulcers. The trilogy of peripheral neuropathy, PAD and susceptibility to infection are the main predisposing factors for lesions on the foot. Other factors that increase the risk include poorly fitting or poor quality shoes, not washing regularly or thoroughly or not drying the feet well after washing, improper trimming of toegether that leads to skin breakdown. Of all the risk factors for DFU the most important is a past history of ulceration and/or amputation. DFU is most common in older men.
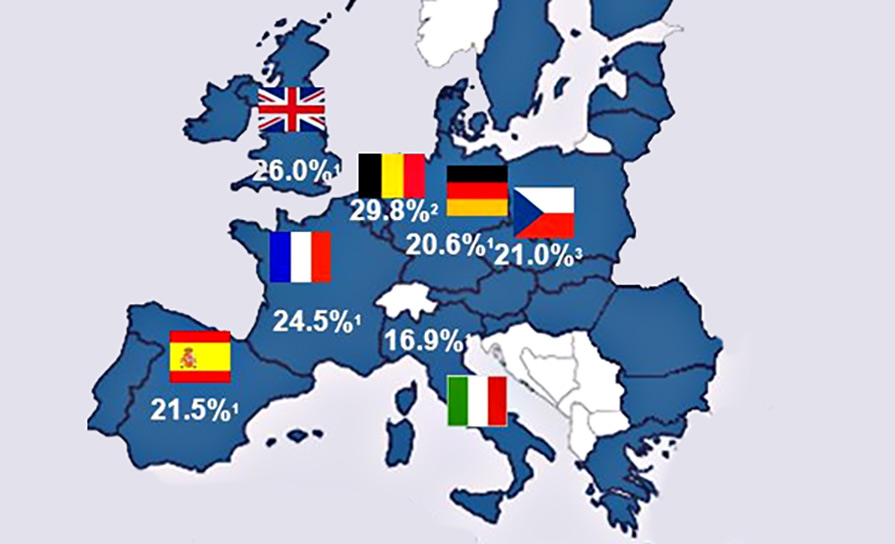
It is estimated that 19-to-34 per cent of patients with diabetes are likely to be affected by DFU in their lifetime, and the International Diabetes Federation reports that 9.1-to-26.1 million people will develop DFU annually. A UK population-based cohort study demonstrated that the development of DFU is associated with a 5 per cent mortality in the first 12 months and a 42 per cent mortality within five years. Patients with DFU were also found to have a 2.5-fold increased risk of death compared with their diabetic counterparts without foot wounds.Effective glycaemic control reduces the incidence of DFU and decreases the risk of amputation. In assessing glycaemic control the HbA1c test should be performed routinely in all patients with diabetes.HbA1c is an indirect measure of average glycaemia and has a strong predictive value for diabetes complications. A target of 53mmol/l (7 per cent) or below is recommended as the optimal target for diabetes patients.Self-monitoring of blood glucose (SMBG) allows real time measurement of blood glucose levels for individuals.
It is important for patients who are self-monitoring to have a good understanding of glucose levels, what their targets are, how well they are achieving this and to play an active role in managing and tailoring their levels and preventing complications
Routine diabetes foot screening should ensure that all patients with diabetes are offered annual screening and regular foot examinations from early diagnosis. Foot review and screening is carried out by appropriately trained staff and foot care education is provided to individuals according to their clinical and personal needs. Patients are regularly assessed for their risk of DFU and classified as low, at risk (moderate or high risk), or with active foot disease.
Foot care management in diabetes is based on three categories of risk
- Patients at low risk of diabetic foot disease are managed preventatively through annual screening and regular foot examinations by primary care nurses. A low-risk patient has normal foot pulses, normal vibration and sensation to 10g monofilament, no history of foot ulceration, no significant foot deformity, or no visual impairment.
- Patients at risk of diabetic foot disease may be classed as either moderate or high risk. All patients will be under regular surveillance by primary care nurses/GPs. Moderate-risk patients will be referred to the podiatrist, either in the community or in the hospital, for an annual review and these patients will remain under the clinical governance of the GP and podiatrist. The moderate-risk patient has either impaired peripheral sensation or impaired circulation or significant visual impairment or a structural foot deformity. High-risk patients will be reviewed at least annually by the diabetes foot protection team in one of the 16 designated centres and will be under the governance of the foot protection team for their foot care. The high-risk patient has an abnormality that predisposes them to foot ulceration. This can be impaired sensation and impaired circulation, or a previous foot ulcer, previous lower limb amputation or previous Charcot foot.
- Patients with active diabetic foot disease have an active foot ulcer (full thickness skin break) or a Charcot foot and will be actively managed by a multidisciplinary specialist foot care service, in conjunction with vascular surgery, orthopaedics, and orthotics input as required. This is available in the eight Model 4 indicative hospitals. The HSE National Model of Care states that patients with active DFU should be referred to the multidisciplinary diabetic foot team (MDFT) in the Model 4 hospital within one working day. Diabetic foot care involves a multidisciplinary team approach including a wide range of professionals as well as patients and their carers. Central to diabetes foot
care are patients, carers, podiatrists, general practice nurses and other primary care nurses, GPs, diabetes specialist nurses, diabetes consultants, orthoptist, vascular surgeons, and orthopaedic surgeons. Other groups with an important input into diabetes foot care are tissue viability nurses, physiotherapists, infectious disease service, radiology consultants, ward nurses, and emergency department (ED) staff.
Screening and assessment Low-risk foot:
Patients previously classified as low risk or patients newly diagnosed with diabetes mellitus should receive annual foot screening as part of their general diabetes care and have the following foot examination.
Diabetic foot care involves a
multidisciplinary team approach
including a wide range of professionals
as well as patients and their carers
Inspection of skin, nails and for structural foot deformity.Vibration perception testing (128Hz tuning fork) and cutaneous pressure perception testing using the 10g monofilament.Palpation of foot pulses.Examination of footwear.
Foot care education involves:
Nail care.Emollient use.Footwear.Daily self-examination of the feet.Not walking in bare feet.Checking footwear and hosiery before putting them on.Breaking shoes in should never be attempted.No hot water bottles.Checking bath and shower temperature.Avoidance of home remedies, eg, corn plasters.What to do and the appropriate person to contact if foot problems develop.A low-risk foot information sheet should be provided.A patient with low risk of diabetic foot disease does not routinely need to see a podiatrist for diabetes-related purposes.
Moderate-risk foot:
A patient at moderate risk of foot complications has either a reduction in vibration or 10g monofilament sensation or has absent foot pulses in either or both feet. There must be no history of ulceration and no significant foot deformity.Foot examination frequency requires ongoing review by GP/general practice nurse or primary care nurse or hospital diabetes clinic as part of routine follow-up. Annual podiatry review by the specialist podiatrist is based either in the community or in the hospital. Patients previously classified as moderate risk should have the following foot examination:
Inspection for structural foot deformity.Skin and nail examination.Vibration perception testing (128 Hz tuning fork) and cutaneous pressure perception testing using the 10g monofilament.Palpation of foot pulses. A comprehensive vascular assessment where indicated, including Doppler waveform analysis, ankle brachial index, and toe brachial pressure index calculation.Examination of footwear
Management
If there is loss of vibration and 10g monofilament sensation the patient should be educated on how to protect their feet. If there is intact sensation and absence of foot pulses in either or both feet, the patient may require further vascular assessment, particularly if there are symptoms of vascular insufficiency. Foot deformity may not need any action, but if it is severe the patient should be referred for specialist assessment. Podiatry advice, biomechanical assessment and discussion of all treatment options including accommodative footwear and orthoses should be provided where required. In some cases orthopaedic surgery may be required.If there is other foot pathology such as nail conditions, corns, callus or verrucae, these can be dealt with during the examination by the podiatrist and a referral to a community podiatrist should be made.Foot care education as previously described should be provided for the patient
High-risk foot:
A patient with high risk of foot complications has both a reduction in vibration and monofilament sensation and PAD –absence of foot pulses. If there is a previous history of ulceration, lower limb amputation or Charcot neuro-arthropathy then the foot is classified as high risk automatically and remains in the high risk category. Foot examination frequency requires ongoing review by GP/primary care nurse/hospital diabetes team. Patients will be called for formal annual review or more frequently as required by the members of the foot protection team or service where appropriate.Patients classified as high risk should have the following foot examination:
Inspection for structural foot deformity.A comprehensive neurological assessment.A comprehensive vascular assessment where indicated, including Doppler waveform analysis, ankle brachial and toe brachial pressure index calculation.Examination of footwear
Management
The diabetes foot protection clinic should take place on a monthly basis at minimum, within the Model 3 or Model 4 hospital and should have input from a diabetes specialist, podiatrist, and diabetes nurse with input where necessary from vascular, orthopaedics, and orthotics.
Podiatrists within the foot protection team or foot care service should review the high-risk foot at least once every 12 months. If ulceration is present the patient should be referred within 24 hours or the next working day to the multidisciplinary foot care service (Model 4 hospital).
The educational needs of the patient should be reviewed.If there is a problem with footwear, the patient should be referred to a podiatrist/ orthotist for footwear assessment and orthoses provision.
The patient should be referred to vascular services. If there is other foot pathology such as nail conditions, corns, callus or verrucae, referral to a community podiatrist should be made.
The hospital podiatrist will work closely with the community podiatrist in the joint care of high-risk foot patients.Foot care education as previously described should be provided for the patient
Active foot disease:
All diabetes patients with an active foot ulcer or active Charcot foot should be referred to the diabetes foot clinic urgently and patients should be seen within 24 hours or on the next working day by the diabetes multidisciplinary foot care service, and involve the appropriate specialties. Patients will be seen weekly by a member of the multidisciplinary foot care service until healing of the ulcer occurs and will be seen regularly in the specialist multidisciplinary foot care clinic until ulcer healing or the Charcot foot becomes stable and inactive.Patients with active foot disease should have the following foot examination:
Inspection for structural foot deformity.
A comprehensive neurological assessment.
A comprehensive vascular assessment where indicated, including Doppler waveform analysis, ankle brachial, toe
brachial pressure index calculation and/ or radiological imaging of the lower limb vasculature.
Radiology investigations where indicated including foot x-ray or MRI of the foot. Isotope bone scan may also be used in certain circumstances.
Examination of footwear.
Management
The diabetes foot care clinic should take place on a monthly basis at minimum, with in the Model 4 hospital and should have input from a diabetes consultant, senior podiatrist and diabetes nurse with input where necessary from vascular, orthopaedics, orthotics, tissue viability, physiotherapy, plastic surgery, and infectious disease.
Podiatrist within the foot care service should review the active foot disease patient at least weekly until healing occurs.
Review the educational needs of the patient.
Referral to a podiatrist/orthotist for footwear assessment and orthoses provision if required.
Refer to vascular and/or orthopaedics where necessary.
If there is other foot pathology such as nail conditions, corns, callus or verrucae, referral to a community podiatrist should be made.
If there are clinical signs of infection, antibiotics should be commenced immediately.
If there are clinical signs of severe/ limb-threatening infection then the patient should be admitted urgently for intravenous antibiotic therapy.
If there is evidence or suspicion of osteomyelitis the patient should be referred for radiological and orthopaedic review.
Control vascular risk factors.
Once the foot ulcer has healed and appropriate footwear organised for the patient, they can be moved back to the ‘highrisk group’ in the ‘at-risk’ category. However, if there is the likelihood of re-ulceration the patient should continue to attend the multidisciplinary foot care service in a Model 4 hospital.
The high-risk foot information sheet should be given to the patient.
A comprehensive assessment of the patient’s general health, glycaemic control, extent of peripheral neuropathy and detailed dermatologic and musculoskeletal examination are included in the evaluation. Clinical evaluation of the foot wound should include a detailed description of the site, size, and depth of wound. Neuropathic ulcers typically occur in the warm but insensate foot, often under pressure-bearing areas, and are surrounded by callus. Ischaemic wounds tend to occur in the cool, poorly perfused foot and are often at lateral fifth metatarsal head regions or the medial
first metatarsal head regions. Correct identification of the degree of ischaemia is of great importance when evaluating a wound.
Classification
Ulcers are graded using the University of Texas Classification System (Figure 2), which is a validated tool specifically for diabetic foot ulcers. The Meggitt-Wagner grading system was regarded as the gold standard for many years. One problem with the Meggitt-Wagner grading system is that the ischaemic status of the wound is not included and therefore a number of new classification systems for diabetic foot wounds have been proposed and validated over the last 20 years. The University of Texas Classification System incorporates the Meggitt-Wagner grades, but also enables the practitioner to stage the wound with respect to the presence or absence of infection and/or ischaemia.
Treatment and management
Depending on the primary underlying cause of ulceration, the wound will be assessed and a management plan will be developed. The management of DFU is multifaceted and combines revascularisation, infection management, debridement of dead tissue and offloading of pressure in addition to hyperglycaemic treatment and wound care.
Treatment of hyperglycaemia, ketoacidosis, renal insufficiency and other comorbidities that may coincide in the ulcerated patient should be treated simultaneously with the foot lesion. Debridement is important as it reduces devitalised tissue, promotes proliferation, granulation, and epithelialisation, eliminates potential pathogens, allows exudate drainage, reveals the true extent of ulceration and reduces pressure on subcutaneous tissue.
DFU should heal if there is an adequate arterial inflow, infection is aggressively managed, and pressure is removed from the wound and its margins. Pressure reduction is essential for a patient who has just been treated for a diabetic foot and off-loading or reducing the pressure plays a significant role in managing the healing process. There are
various off-loading modalities such as the total-contact casts (TCC), removable cast walkers (RCW) and half shoes, and studies have been conducted to compare their effectiveness to heal neuropathic foot ulcerations in diabetic individuals. Although less commonly used, results reveal that TCC is better and heals a comparatively higher number of
wounds in a shorter duration of time. In the management of plantar neuropathic ulcers, offloading is critical and all efforts must be made to enhance patient understanding of the need for offloading.
Identification of infection in wounds can be challenging and particularly so in DFU. In the presence of neuropathy and ischaemia, signs of infection can be diminished as the normal inflammatory response is impaired. The correct diagnosis of infection in the diabetic foot wound is critical as it is often the combination of untreated infection and PAD
that lead to amputation in the diabetic foot. If osteomyelitis is suspected plain x-rays can assist diagnosis, however, initially reports may prove normal and evidence of osteomyelitis may not be apparent for 14 days. Antibiotic usage should be guided by clinical signs of infection and microbiologic analysis of deep tissue specimens.
Most adjunctive therapies have little evidence to support their use, although recent trials suggest efficacy for a number of topical therapies including LeucoPatch and sucrose octasulfate. Negative pressure wound therapy has also been shown to be helpful in certain cases. There is currently no indication for hyperbaric oxygen usage, whereas recent
studies suggest that topical oxygen therapies may help wound healing.
Wound dressings are important to keep the ulcer clean, but the placement of a large dressing on a wound may mislead the patient into believing that the dressing of an ulcer is curative. Although there has been much progress in the understanding and management of diabetic foot disorders over the last three decades, much of what we use in clinical practice today still lacks an evidence-base. This is particularly true for dressings and there is little evidence from
randomised controlled trials (RCTs) that any dressing is superior to another.
Prevention and recurrence
Prevention of diabetic foot disease can only be successful with the early identification of patients who have risk factors for foot ulceration. All patients with diabetes should, at whatever stage, be screened for evidence of complications at least annually. The principle aim of the annual review is to identify those with early signs of complications and provide appropriate management to prevent progression. The most important aspect of the annual foot review is the removal of shoes and socks with very careful inspection of both feet including between toes.
Many neuropathic feet can be identified by this simple clinical observation, looking for features such as small muscle wasting, clawing of the toes, prominence of the metatarsal heads, distended dorsal foot pains, dry skin, and callus formation. For evidence of neuropathy, the perception of pressure using the 10g monofilament should be used at four sites in each foot. An additional test, which might include a vibrating 128Hz tuning fork, should also be used to confirm any abnormality. For the vascular assessment, foot pulse palpation is most important. The ankle brachial index may be falsely elevated in many patients with diabetic neuropathy and therefore listening to the Doppler signal may be more helpful.
Other simple devices developed for clinical screening that have been validated in clinical studies include the ‘Ipswich Touch Test’, which assesses the ability of the patient to perceive the touch of a finger on the toes and the ‘Vibratip’, a battery-operated disposable vibrating stylus used to assess vibration sensation. A number of studies are currently
looking at ‘smart technology’ in the prevention of recurrent DFU. These include the use of sensors in socks or shoes to detect pressure change and also various devices to measure differentials in skin temperature. These technologies aim to alert patients in the pre-ulcerative phase with the hope of preventing the actual ulcer from developing.
Recurrence is common after the healing of neuropathic or neuro-ischaemic foot ulcers and the patient is termed in remission rather than healed following an episode of DFU. While the symptoms may have resolved the underlying disease process remains and the symptoms of the disease will likely re-occur. Rates of DFU recurrence are up
to 40 per cent one year following DFU. It is important that patients and their families are educated about the persistence of DFS even in the absence of DFU.
All individuals with diabetes should receive regular screening and structured education to empower them to maintain
their own foot health. Early identification of problems and rapid referral to the specialist multidisciplinary team can reduce the risk of DFU and unnecessary amputations. Foot care programmes accentuating preventive management can reduce the incidence of foot ulceration through modification of selfcare practices, appropriate evaluation of risk
factors and formulation of treatment protocols directed at patient education/re-education, early intervention, limb preservation and prevention of new lesions.
References
- Tuttolomondo A, Maida C, Pinto A. (2015). Diabetic foot syndrome: Immune-inflammatory
features as possible cardiovascular markers
in diabetes. World J Orthop. 2015 Jan 18;
6(1): 62–76.doi: 10.5312/wjo.v6.i1.62 - Wilson P, Fu W, Doyle J. (2021). Joining the
dots … Diabetes mellitus and foot disease.
Irish Pharmacy News, Volume 13, Issue 7, pp
68-69. Available at: www.pharmacynewsireland.com/digital-magazines/ - Rodríguez-Gutiérrez R, Quintanilla-Flores DL,
Soto-Garcia AJ, Gonzalez-Gonzalez JG, Sieradzki J, Płaczkiewicz-Jankowska E. Diabetic
foot syndrome. McMaster Textbook of Internal
Medicine. Kraków: Medycyna Praktyczna.
https://empendium.com/mcmtextbook/
chapter/B31.II.13.4.4 - Healthline (2021). Diabetic Ulcers: Causes and Treatment. Available at: www.
healthline.com/health/type-2-diabetes/
hyperglycemic-hyperosmolar-syndrome - Everett E, Mathioudakis N. Update on
management of diabetic foot ulcers. Ann
N Y Acad Sci. 2018 Jan; 1411(1): 153– - doi: 10.1111/nyas.13569
- Boulton A, Whitehouse W. (2020). The Diabetic Foot. NCBI. Available at: www.ncbi.nlm.nih.
gov/books/NBK409609/ - HSE (2011). Model of care for the diabetic
foot. HSE Available at: www.hse.ie/eng/
services/list/2/primarycare/east-coast-diabetes-service/management-of-type-2-diabetes/
foot-care/model-of-care-diabetic-foot.pdf - Diabetes Ireland (2021). Know your numbers
and targets. Diabetes Ireland. Available at:
www.diabetes.ie/are-you-at-risk-free-diabetestest/a-numbers-game/ - NUI Galway (nd). Foot screening and education of the patient with diabetes. Discipline
of Podiatry School of Health Sciences NUI
Galway. Available at: www.hse.ie/eng/services/publications/clinical-strategy-and-programmes/foot-screening-and-education-of-the-patient-with-diabetes.pdf - Niederauer M, Michalek J, Liu Q, et al. (2018).
Continuous diffusion of oxygen improves diabetic foot ulcer healing when compared with a
placebo control: A randomised, double-blind,
multicenter study. J Wound Care. 2018;
27 suppl 9:S30–S45











Leave a Reply
You must be logged in to post a comment.