Cystitis is a common presentation in women, which can usually be diagnosed and managed in general practice,
but onward referral to a urologist is sometimes necessary
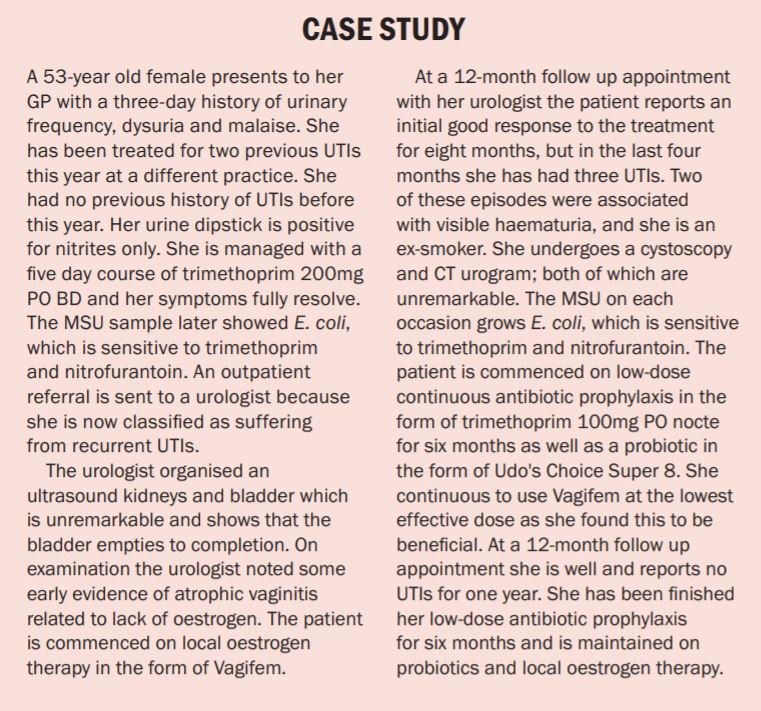
Cystitis is defined as an infection and/or inflammation of the bladder. The presentation may involve frequent voiding of small volumes of urine, dysuria, urgency, odorous urine, suprapubic pain, haematuria, urinary incontinence or fever. Cystitis in the presence of infection may be classified as a urinary tract infection (UTI). An uncomplicated UTI is one occurring in a structurally and functionally normal urinary tract. This type of UTI accounts for the majority of cystitis cases in female patients and will typically resolve with a short course of antibiotics.
Cystitis may also occur in the absence of a UTI. There are three main causes for non-infectious cystitis. It may occur after pelvic radiotherapy and is often referred to as radiation cystitis. It may also occur if the patient has a history of cyclophosphamide or ketamine use. Interstitial cystitis (or more recently known as bladder pain syndrome) is a chronic debilitating disorder with similar symptoms to infectious cystitis, but is diagnosed by excluding all other causes.
Risk factors and aetiology
Risk factors for cystitis in females include; increasing age, reduced oestrogen (menopause), previous UTI, diabetes mellitus, pregnancy, institutionalised elderly patients, stone disease, indwelling catheters, voiding dysfunction and genitourinary tract malformation. Risk factors in pre-menopausal patients include sexual intercourse, use of spermicide, new sexual partner, history of childhood UTI, and mother with a history of UTI.
The most common causes of cystitis are Escherichia coli (E. coli), a Gram-negative bacillus, which accounts for 85 per cent of community-acquired and 50 per cent of hospital-acquired cystitis infections. Other common causative organisms include Staphylococcus saprophyticus, Proteus mirabilis, and Klebsiella. Bacteria from the bowel colonise the perineum, vagina, and distal urethra. From here the bacteria ascend along the urethra and reach the bladder causing cystitis.
Investigations
The first investigation for cystitis should be a urine dipstick, which has several components to interpret. Leukocyte esterase activity detects the presence of white blood cells (WBCs) in the urine. The presence of WBCs in the urine is referred to as pyuria and implies an inflammatory response of the urothelium (lining of the bladder) to a bacterial infection. This component of the urine dipstick has a sensitivity of 75-to-95 per cent for detection of infection. The next component is nitrites.
These are not normally found in the urine and their presence suggests there is bacteria in the urine (bacteriuria). The sensitivity of this test is only 35-to-85 per cent (false negatives are common), but if nitrites are positive on a dipstick then it is highly likely there is an infection because the specificity is very high (>90 per cent). A mid-stream urine (MSU) sample, which is collected for a dipstick test, may also be sent to a lab for microscopy and culture. False positives on microscopy may occur due to vaginal commensal bacteria, such as lactobacillus and Corynebacterium. To make a diagnosis of an uncomplicated UTI it is recommended that a urine culture would demonstrate >103 colony forming units per millilitre (cfu/mL).
Usually a solitary episode of cystitis does not require any further investigations. However, further tests such as renal ultrasound, cystoscopy or CTKUB (kidney, ureter and bladder) may be necessary in certain clinical scenarios such as recurrent UTIs, unusual organisms on MSU, pregnancy or symptoms of pyelonephritis. Ultrasound may detect hydronephrosis, renal calculi, or structural abnormalities, and can be used to calculate the post-void residual volume in the bladder. CTKUB may detect renal, ureteric or bladder calculi. Cystoscopy may detect rare causes of recurrent UTIs such as urethral stenosis, bladder cancer, bladder calculi or a fistula.
Management
Acute cystitis episode
For acute uncomplicated cystitis, treatment with one of the following regimens is recommended: Nitrofurantoin 50mg PO QDS for five days, trimethoprim 200mg PO BD for five days, or fosfomycin 3g PO single dose for one day. Acute cystitis episodes may also be prevented with general measures such as good fluid intake, avoiding constipation, cranberry juice, double voiding and wiping from front to back after voiding.
Recurrent UTIs
Recurrent UTIs are defined as >two infections in six months or three within 12 months. For recurrent UTIs, the European Association of Urology (EAU) guidelines panel recommends offering either three-to-six months of continuous low-dose antibiotic prophylaxis or post-coital antibiotic prophylaxis (single dose only). Continuous low-dose regimens include nitrofurantoin 50-to-100mg PO nocte, trimethoprim 100mg PO nocte, or fosfomycin 3g every 10 days.
Patients with good compliance should be offered self-diagnosis and self-treatment with a short-course regimen of antibiotics (the same regimens we discussed for acute cystitis episodes) for recurrent UTIs. It is important to avoid using unnecessarily long courses (>five days) of antibiotics for acute cystitis episodes in this group of patients in order to prevent reduced efficacy of antibiotics.
There are a number of treatment measures for UTIs besides antibiotic prophylaxis – effective lifestyle modification, particularly while at work, including avoiding habitual delayed urination and maintaining good fluid intake. It is important to avoid the spermicides that are present on condoms and the diaphragm. Post-menopausal women have a lack of oestrogen resulting in loss of protective lactobacilli. Topical oestrogen replacement with products such as Ovestin or Vagifem, but not oral oestrogen, has been shown to be effective at reducing recurrent UTIs.
Proanthocyanidin (PAC) contained in cranberry products block bacteria adhering to the lining of the urinary tract and consumption of cranberry products has been shown to reduce the absolute risk of UTIs by 20 per cent. Applying natural yoghurt to the vagina may help to restore the natural protective flora. Probiotics (lactobacillus) are generally regarded as effective at reducing recurrent episodes of cystitis, however, studies have failed to demonstrate this benefit. Udo’s Choice Super 8 is an example of a probiotic that is commonly recommended by urologists and is available without prescription.
D-Mannose is a product which can also be purchased without prescription and it has been shown that taking 2g of the powder dissolved in 200ml water daily reduces the risk of UTIs by 45 per cent. D-Mannose is thought to work in a similar manner to cranberry products by blocking the binding of bacteria to the urothelium. In diabetic patients with recurrent cystitis it is important to improve glucose control to reduce the frequency of episodes. Courses of Hiprex 1g PO OD have been shown to reduce UTI episodes, but it is not commonly used.
The efficacy of acupuncture has been investigated for recurrent UTIs, and in a small series it was shown to be more effective than placebo, but there is not strong enough evidence to recommend it as a treatment. Administration of hyaluronic acid (iAluril) into the bladder once per week for four weeks has been investigated for recurrent cystitis. A small series showed an 86 per cent reduction in UTI episodes. This treatment option appears from small studies to be effective, but is costly to administer in terms of healthcare resources.
Conclusion
In summary, cystitis is a common condition in females which can be diagnosed with clinical history, examination and mid-stream urine collection. It is typically caused by E. coli from the bowel which colonises the perineum and vagina, and ascends the urethra to cause cystitis. Acute episodes should be treated with appropriate short-course antibiotics and patients given information on general preventative measures. No further investigations are required in one-off uncomplicated UTI episodes.
Recurrent UTIs warrant referral to a urologist for further investigation, which may include imaging and cystoscopy to exclude structural or functional urinary tract abnormalities or underlying bladder pathology. Management of recurrent cystitis varies by age, but includes continuous low-dose prophylactic antibiotics, post-coital antibiotic prophylaxis, lifestyle modifications, topical oestrogen, cranberry products, probiotics, and D-Mannose.
References on request










Leave a Reply
You must be logged in to post a comment.