HOW OFTEN do you meet a patient who describes symptoms of urinary tract infection (UTI), but the urinalyses, whether dipsticks or culture, prove negative? Have you noticed the increasing numbers of predominantly women who keep re-presenting with lower urinary tract symptoms (LUTS) that defy the advice of the tests that you use? You are doing right by the guidelines and you have taken note of the contemporary concerns about antimicrobial resistance (AMR). These patients are baffling aren’t they?
The specialists write about ‘painful bladder syndrome’ (PBS), renamed ‘bladder pain syndrome’ (BPS) or ‘interstitial cystitis’. So, the patients are ultrasounded, CT and MRI scanned. They are urodynamicked, cystoscoped, bladder-stretched, urethra-dilated, and then instilled with various concoctions, but frustratingly still they return.
This perplexing problem has been my obsession for forty years, and with our happy gang of researchers it would seem that we have come up with some useful answers. Today we have sufficient knowledge for me to write a book about it, Cystitis Unmasked, that is pitched at clinicians and informed patients alike. There is quite a story because our science found that the guidelines and urinalyses methods were incorrect. That is a gentle adjective because the truth is that they are calamitously wrong. However, we have learned that reporting such science to power is a tricky business.
We have spent a decade deflecting a string of criticisms by the chaps in charge who seemed outraged by the outcomes of our science. Feelings ran so high that we felt obliged to conduct the studies necessary to address every proposition that was floated to explain away what we were trying to report. Thus, we evaluated one ‘no true Scotsman’ argument after another in a dispiriting sequence of negative experiments. However, today I may report that the original findings have weathered a hugely detailed critical scrutiny, so we have some confidence in what we have published.
The dipstick test1 and the urine culture2,3 are grossly unreliable witnesses of the events extant in the urinary tract. To dismiss the diagnosis of UTI, despite appropriate symptoms, because one or both of these tests are negative, is a serious fallacy, with the technical term of ‘ignoring the base rate’. The scientific truth is that if the patient has symptoms the probability of a UTI is high indeed and a negative test is probably a false negative.
The normal bladder is not sterile, but hosts a complex polymicrobial microbiome of several hundreds of different species, and a 95 per cent overlap with patients who have UTI.5 There is no truth in the claim that the microbe isolated by a midstream urine culture (MSU) is the proven causative organism. The problem of causation is unresolved and applies equally to enhanced cultures and genomic methods.
We may isolate microbe(s) but we haven’t a clue whether they are friend or foe. If you treat on the sensitivity data obtained from a culture you are more likely to fan the flames of AMR than treat the patient successfully.6,7 Simple, narrow-spectrum, urinary antibiotics in sufficient dose will perform just as well with less AMR. ‘Mixed growth of doubtful significance’ is of considerable significance in reflecting the pathology of UTI.2 The epithelial cells identified in urinalyses are not indicators of contamination, but important biological manifestations of active cystitis.8
It is not just the testing that is in such a parlous state; the treatment guidelines are equally dubious. Three-day and 14-day courses of antibiotic for acute UTI carry a 25-to-35 per cent failure rate9 yet the advice is that you should manage such unfortunates using a discredited culture.10
This is all most worrying. The science has been done carefully and additional work has been achieved to address the common arguments that have been used to claim that none of this could be true. The time has come for those who have the relevant influence to insist that the guidelines and regulations should be re-examined in the light of this new knowledge. It is most unfair on the patients to do otherwise.
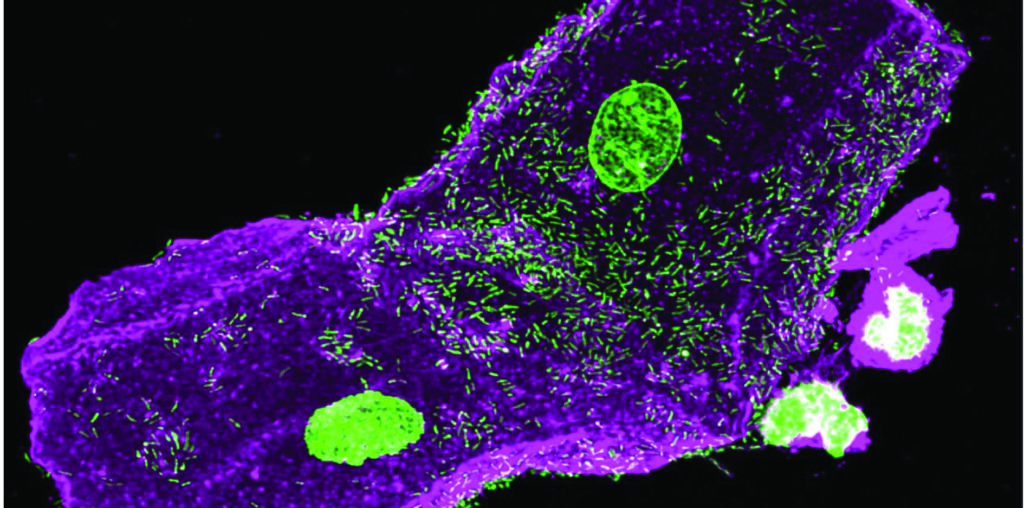
To conclude, please consider two images. The first is a confocal micrograph (Figure 1) achieved by Dr Harry Horsley PhD, a most gifted researcher in our centre. It shows urothelial cells extracted from a urine sample and reveals microbes adherent to the surfaces of these cells, but others parasitising these unfortunate cells in order to set up a chronic infection that will be hard to eradicate. This is the pathology that explains those patients who keep returning to you with recalcitrant symptoms but negative tests.
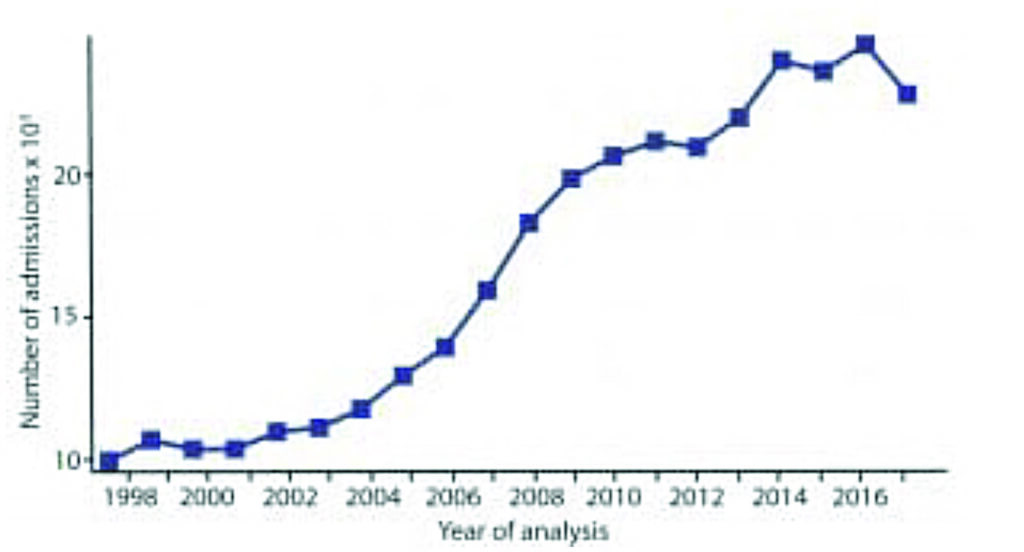
The second is the graph (Figure 2) of the NHS returns for admissions for IC/PBS/BPS annually since 1998. The outpatient attendances paint a similar picture. There is a most worrying rise in the incidence. It started in 2002 and that follows the publication of the first guidelines stipulating three-day antibiotic courses for acute UTI. We do not know whether adherence to those restrictions is the cause of this phenomenon, but that science supports such an hypothesis is certainly worth thinking about.
Prof Malone-Lee’s book is Cystitis Unmasked. TFM Publishing Ltd (1 February 2021). His author royalties will be donated to the current research programme at UCL.
This article first appeared in BMJ Life (https://bjgplife.com/2021/03/19/confronting-the-urinalysis-tyrant/) and was reproduced with kind permission from the author and Editor.
References
- Kupelian AS, Horsley H, Khasriya R, Amussah RT, Badiani R, Courtney AM, et al. Discrediting microscopic pyuria and leucocyte esterase as diagnostic surrogates for infection in patients with lower urinary tract symptoms: Results from a clinical and laboratory evaluation. BJU Int 2013; 112(2): 231-8
- Sathiananthamoorthy S, Malone-Lee J, Gill K, Tymon A, Nguyen TK, Gurung S, et al. Reassessment of routine midstream culture in diagnosis of urinary tract infection. J Clin Microbiol 2019; 57(3): 01452-18
- Gill K, Kang R, Sathiananthamoorthy S, Khasriya R, Malone-Lee J. A blinded observational cohort study of the microbiological ecology associated with pyuria and overactive bladder symptoms. Int Urogynecol J 2018; 29(10): 1493-500
- Khasriya R, Barcella W, De Iorio M, Swamy S, Gill K, Kupelian A, et al. Lower urinary tract symptoms that predict microscopic pyuria. Int Urogynecol J 2018; 29(7): 1019-28
- Hilt EE, McKinley K, Pearce MM, Rosenfeld AB, Zilliox MJ, Mueller ER, et al. Urine is not sterile: Use of enhanced urine culture techniques to detect resident bacterial flora in the adult female bladder. J Clin Microbiol 2014; 52(3): 871-6
- Swamy S, Barcella W, De Iorio M, Gill K, Khasriya R, Kupelian AS, et al. Recalcitrant chronic bladder pain and recurrent cystitis, but negative urinalysis: What should we do? Int Urogynecol J 2018; 29(7): 1035-43
- Swamy S, Kupelian AS, Khasriya R, Dharmasena D, Toteva H, Dehpour T, et al. Cross-over data supporting long-term antibiotic treatment in patients with painful lower urinary tract symptoms, pyuria, and negative urinalysis. Int Urogynecol J 2019; 30(3): 409-14
- Horsley H, Malone-Lee J, Holland D, Tuz M, Hibbert A, Kelsey M, et al. Enterococcus faecalis subverts and invades the host urothelium in patients with chronic urinary tract infection. Plos One 2013; 8(12): e83637
- Zalmanovici TA, Green H, Paul M, Yaphe J, Leibovici L. Antimicrobial agents for treating uncomplicated urinary tract infection in women. Cochrane Database Syst Rev 2010; (10): CD007182
- NICE. Urinary tract infection (lower) – women. London: National Institute for Health and Care Excellence, 2014. Available from: http://cks.nice.org.uk/urinary-tract-infection-lower-women#!topicsummary













Leave a Reply
You must be logged in to post a comment.