Is adolescent and transitional urology a healthcare right or a privilege?
Case report
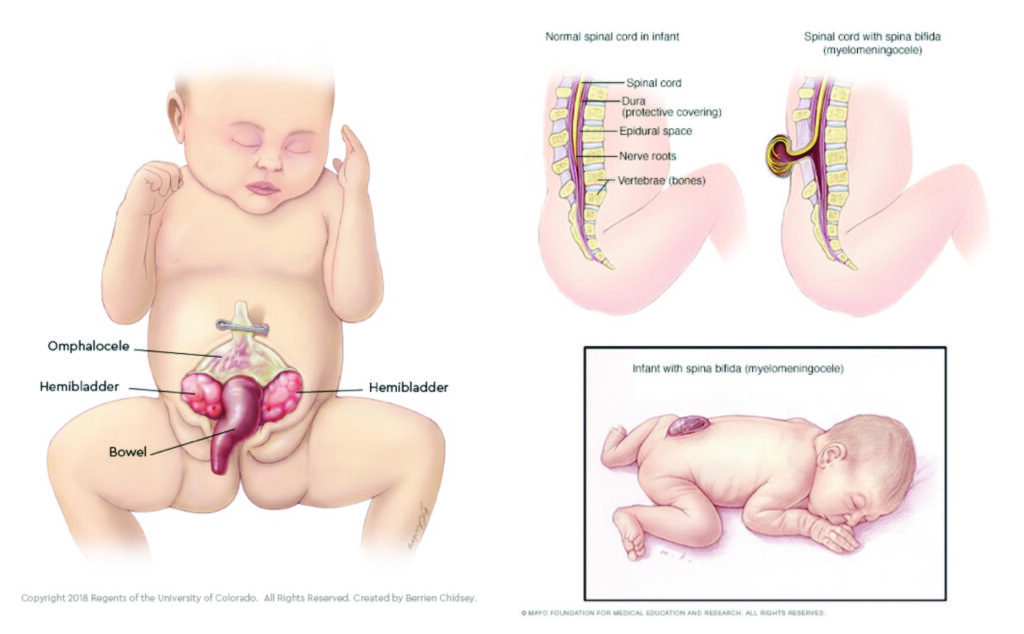
Joe Holliday was born with cloacal exstrophy in 1988. Due to the devastating nature of this condition, he had ambiguous genitalia, and an inguinoabdominal gonad. It was felt at the time that it would be psychologically damaging for him to be raised as male, and therefore was raised as female from the age of one. His name, and sex were legally changed in 1998 in a landmark case. Joella’s unhappiness continued throughout adolescence as she felt different from other girls, and was also on hormonal medication. She had recurrent episodes of suicidal ideation. At the age of 25 she ordered a karyotype, which demonstrated her to be genetically male, and at 27-years-old, she transitioned back to being male.
Historical context
Historically, the majority of children with major congenital anomalies died at a young age. Half (50 per cent) of those born with classic bladder exstrophy died by the age of 10 years before the 1950s. There were no survivors of cloacal exstrophy until the 1960s and the majority of those born with spina bifida failed to survive beyond infancy.
There was no treatment for end-stage renal failure until dialysis in the 1960s, and 50 per cent of boys born with posterior urethral valves routinely died before reaching adulthood. Antibiotics designed to combat gram-negative infections were only discovered in the 1970s, which meant that bacteraemia (especially that in conjunction with renal tract stones) had a very high mortality rate.
There were few long-term survivors, and therefore need for long-term urologic congenital care, until the 1970s at the earliest. With improving survival rates in the second half of the 20th century due – in no small part – to improvements in anaesthesiology, microbiology, critical care medicine and paediatric physicians, it was realised that many children with congenital anomalies would require long-term, holistic, medical and surgical care. In Europe and Australia, some early special units to cater to adolescent urological conditions appeared in paediatric hospitals. These were also established in Canada such as in the Hospital for Sick Children (SickKids), Toronto. This never happened in Ireland.
Societal contributions
Patients with congenital anomalies, like the rest of the population, want to have the opportunity to live a normal adult life. Most of these patients are able to grow, develop, and make high-level contributions to society. In a 2012 paper by Woodhouse et al, 65 per cent of patients with a range of congenital anomalies were employed in skilled, administrative, or professional roles.
What is transitional urology?
Adolescence is perceived as the phase of passing from childhood to adult life. The OED (Oxford English Dictionary) defines it as between childhood and manhood (14-25 years old), and womanhood (12-21 years old).
Transitional urology in itself is a multi-faceted process designed to facilitate a patient who is able to accept full responsibility for medical decision-making and care, to move to an adult urological care team. The majority of groups, such as the International Consultation on Urological Diseases, recommend beginning the process of transition at around 12 years old (or earlier).
This is to provide ample time for all parties involved to develop the skills and understanding required by the age of 16 to 18 years old, depending on the jurisdiction, which in Ireland is 16 years. The goal of transition is to provide uninterrupted, developmentally appropriate transfer of medical care to an adult care model.
The main difference in models of care is that the paediatric model involves a large team from different disciplines, led by a single surgeon. The care approach is usually parent-focused with longer consultation times, good access to psychology and regular follow-up appointments. The adult model is generally a smaller team with sub-specialty interests requiring more outside consultation. The care approach is patient-focussed, with shorter consultation times, less availability of psychology, and longer review intervals.
The typical patient case-mix seen in adolescent and transitional clinics include, but is not limited to, the following:
- Bladder: Neurogenic bladder (including myelomeningocele; CNS injury); urinary diversion; exstrophy.
- Renal: Renal anomalies; vesicoureteric reflux; posterior urethral valves; Prune belly syndrome; VACTERL.
- Genital and sexual conditions: Epispadias; hypospadias; congenital adrenal hyperplasia; disorders of sexual development.
- Gender dysphoria and those seeking gender transition.
- Oncologic surveillance: Testicular, renal and other childhood/adolescent malignancies.
In addition to addressing the direct urological issues associated with each of these conditions, there are a number of important adjuncts in the lives of these patients which equally require management. This period is one of great social and emotional lability. It is associated with the emergence of sexual function, fertility, sexuality, integration, work life, and independence. It is also associated with the establishment of continence, identity, family integration, and community living.
There are a number of important considerations when managing transitional urology patients, which require a holistic multidisciplinary approach including urology, nephrology, gynaecology, endocrinology, medical genetics, psychology and social work. The aims prior to attending adult services as described by Timberlake et al (J Pediatr Urol 2015; 11(2):62.e1-6) are to:
- Participate independently in their own care.
- Establish familiarity and comfort with adult physicians and nurse providers.
- Obtain and maintain healthcare coverage, or institutional financial assistance (multipayer systems).
- Attend at least one preventative care visit per annum with an adult provider.
- No delayed or forgone essential visits in the prior year to transition.
Transition of care is an essential aspect of healthcare delivery. There can be a complexity involved in management of certain cohorts (eg, the paediatric exstrophy patient), and a similar approach and infrastructure may be needed when the patient transitions to the adult environment.
We are still learning and evaluating, not only about the long-term outcomes and ramifications of surgical procedures, but also how to set up the infrastructure and obtain resources necessary for transition of these patients into adulthood within our challenging healthcare environment.
Why bother transitioning at all?
There is no silver bullet associated with transitioning care from paediatric to adult services. A study from Indiana, US demonstrated a success rate of only 40 per cent for a spina bifida cohort, however, those that were transitioned were statistically less likely to show up in the emergency department for various issues (Szymanski KM et al. J Pediatr Urol 2017; 13(1):40.e1-40.e6). Another study by Agarwal et al (World J Urol 2019;37(4):607-611) illustrated some of the behavioural barriers to transition including a lack of resources, no available, appropriate adult providers, and actually not believing it to be necessary. They felt that moving forward, guidelines, provider education, collaboration and access would be important in breaking down these cognitive siloes.
Transitional urology in itself is a multi-faceted process designed to facilitate a patient who is able to accept full responsibility for medical decision-making and care, to move to an adult urological care team
However, there are a number of studies which have explored the economic impact of formally transitioning patients from paediatric to adult services. Even within the constraints of social determinants of healthcare including race, background, and location, transitioning patients led to significant cost reductions to outpatient visits, emergency department visits, inpatient costs, and surgical costs (Sheppard CL et al. J Urol 2018; 199(4): 1050–1055). Simply put, failure to transition patients disrupts the ratio of outcomes:costs with worse outcomes, and higher costs. This is the exact opposite of value-based care in any healthcare system.
There are a number of systemic limitations to successful transitioning of urologic care to adult services. These relate to insurance provision and coverage in multi-payer systems such as the US. In countries without a universal health system, lack of insurance coverage is a significant detriment to transition of care. Once patients in such systems reach adulthood, coverage via family or government plans may lapse and insurance coverage can quickly become unaffordable. This thus limits their ability to see providers for preventative health visits, forcing them to delay seeking care until problems progress significantly in severity or acuity. This generally doesn’t stand up to scrutiny in countries with government-backed healthcare access such as Ireland, the UK, or Canada, and the issue becomes one of inertia, ego, public expense accounts, and a lack of outcomes recording.
The SickKids model (Toronto)
Urologic transition in SickKids, Toronto is done in collaboration with Sunnybrook Hospital. It is a multidisciplinary approach which involves urology (paediatric and adult), social work, psychiatry, nurse practitioners, gynaecology, andrology, endocrinology, and nephrology.
They employ a 26-item questionnaire through the department of adolescent medicine (Good 2 Go transition programme) which focuses on the understanding of the adolescent as to their physical, clinical, psychological, and social needs. They also employ a ‘MyHealth 3 Sentence Summary’, which patients are encouraged to express at each visit to help with retention of information, and to focus on specific issues important to them.
The website also holds a variety of other tools, resources, and other helpful websites that are available to youths and their families, and can assist with processes and information about transitioning to the adult system.
The Toronto transition system also concentrates on current living arrangements, key players and stakeholders in the health of the patient, quality-of-life concerns for the patients/caregivers, details of prior treatments or operations, and assessments of:
- Renal function.
- Bladder management.
- Infection history.
- Faecal/urinary continence history and goals.
- Stone history.
- Sexual issues/goals.
- Fertility issues/goals.
What about transitional urology in Ireland?
At present, discharge from paediatric to adult urologic care occurs at 16 years in Ireland, unless there are exceptional, extenuating circumstances. Adult urologists in Ireland are for the most part sub-specialised, and few deal with complex reconstruction, or have experience in any paediatric urologic care. Individual cases are accepted on an ad hoc basis, with no measurement of outcomes or costs. Paediatric general surgeons with a special interest in urology are unable to care for these patients as adults, and adult urologists are unable to care for many of them as they lie outside of a scope of practice. The fear of litigation can also be a significant deterrent. There is little formal communication between both professional groups and the HSE is concerned about spiralling healthcare costs, and the impact that Covid-19 will have had on current waiting lists and resource consumption.
Perhaps professional guidance documents can provide an expression of intent? The Urology – A model of care for Ireland document published by the RCSI and the National Clinical Programmes in Surgery suggest that “there should be two designated lead clinicians for paediatric and adolescent congenital and acquired urological diseases transitioning into adulthood, attached to both the National Paediatric Hospital, and an adult urology unit”. The Improving Services for General Paediatric Surgery document published by the National Clinical Programme for Paediatrics and Neonatology, document that “it matters little whether the surgeon’s main specialty lies within general surgery, urology, or paediatric surgery, so long as the individual has the required competencies”. Unfortunately, the document doesn’t mention “adolescence”, or “transitional care”.
Is this a matter of health equality?
Krieger defines health inequality as “…health disparities, within and between countries, that are judged to be unfair, unjust, avoidable, and unnecessary (meaning: are neither inevitable nor un-remediable) and that systematically burden populations rendered vulnerable by underlying social structures and political, economic, and legal institutions” (Krieger N. J Epidemiol Community Health 2001;55(55):693–700).
Could the lack of access to transitional urology in Ireland be termed as inequality? It is unfair, unjust, avoidable, unnecessary, and a legacy of health economic and political institutions on this island. One of the main catalysts for change must be the measurement of patient-related outcomes in urology and indeed general paediatric surgery. The Bill of Mortality for a
single week in London (1665) provides an example of the changes that could be made here with simple measurements. It is one thing to measure outcomes and claim that there is no money by which to improve them – the techniques and processes available to ameliorate that are legion. It is a very different matter to not measure anything at all. The latter is concerning as it may open health professionals and healthcare systems to a legal challenge on the World Health Organisation (WHO) stance that health is a human right, not a privilege.
How could one go about implementing this?
It would be naïve in the least, to assume that adult services can simply take on all transitional care needs. To date, and in a number of fields, where expertise and resources have not been available, this has led to non-standardised and non-timely care managed with wasted adult resources. Systematic identification and stratification of transitioning patient requirements are paramount, and a dynamic grading system with a heavy weighting on diagnosis would allow physicians and management to predict the level of adult care required.
One possibility is the 1,2,3,4 Transitional Care Framework, which is employed by my former colleagues in SickKids, Toronto. The system there allows for risk stratification, dispels misconceptions about what care is and is not required, allows for financial planning, and routinely measures patient reported outcomes. A modified version of the system could be envisaged below. It characterises between conditions, which are not likely to burden adult care in any way with transition by way of webinars and even discharge to primary care, to those conditions which would likely require life-long specialist care (Modified from Dr D Bagli; SickKids).
Framework 1: Web/education/reference guides; anticipate little/no change to adult care. Framework 2: Nursing/tele-counselling/protocol distribution; anticipate minimal change to adult care. Framework 3: Scheduled nursing visit/physician tele-counselling or as required clinic visits; anticipate light hospital support. Framework 4: Ongoing, lifelong support with clinic appointments/advanced nurse practitioner support/direct access to tertiary paediatric and adult hospitals; anticipate moderate hospital support. Framework 5: Multiple complex conditions/life-long care/requires multidisciplinary input/likelihood of access to operating theatres/interventional radiology/pain management high; anticipate significant resource utilisation and hospital support.
In summary
In summary, urogenital congenital abnormalities are common with contemporary better survival outcomes. Late effects and concerns often emerge after puberty (compliance; changes in physiology; lifestyle). Transitional urology is an emerging sub-subspecialty for extended management of patients with congenital genitourinary anomalies that need long-term care. It must include a multidisciplinary approach with social and psychological support. Adolescent urologists continue care in the adult setting, however, it is important to transition patients to be self-reliant to look after their own urogenital conditions. Ireland is in the position that these expertise are now available, and given that, must be cognisant of the dangers of establishing a precedence in health inequality.













Leave a Reply
You must be logged in to post a comment.